|
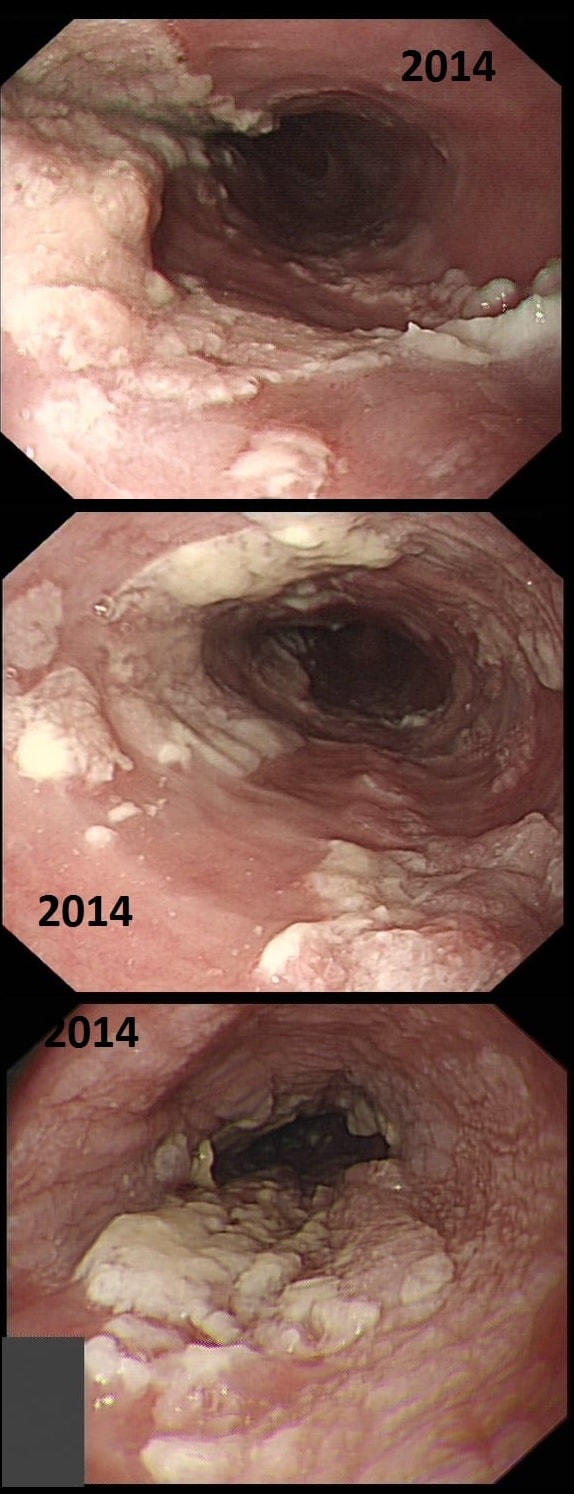
This patient presented with odynophagia and this is the appearance of the oesophagus from 2014
WHAT WAS THE INITIAL DIAGNOSIS IN 2014 ?
■ Candidiasis
These lesions or to 'fleshy'!
■ Reflux oesophagitis
The lesions are too 'fleshy'!
■ Eosinophilic oesophagitis
Doesn't explain the 'lumpiness' of the mucosa
■ Oesophageal papilloma
A papilloma gone mad !
explanation
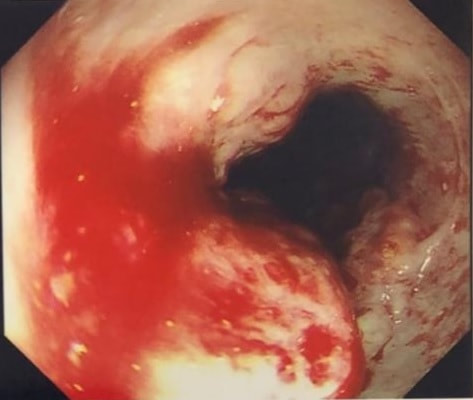
This is a case from Pradeep Mundre at Bradford. The correct diagnosis was 'Diffuse oesophageal Squamous papillomatosis'. Unfortunately, by 2021 the patient re-presented with worsening symptoms was was found to have developed a 'basaloid squamous cell carcinoma' (photo below).
Squamous Papillomas and Squamous papillomatosis of oesophagus Papillomas are finger-like projections that histologically have a central fibrovascular core surrounded by proliferative squamous epithelium with keratin outside this. Of course these are usually small and isolated. However they can become larger and rarely there is diffuse changes as in this case, and term 'oesophageal papillomatosis' is applied. There is little in the published literature on oesophageal papillomas with just a few published case series. Aetiology is unclear as to why some grow large whilst the vast majority remain tiny. Published literature has been conflicting with regards to association of oesophageal papillomas with HPV infection. Clinical relevance, natural history and whether this is a premalignant lesion, remain a matter of debate. There has been a few case reports of progression/ association with squamous cell carcinoma, especially with diffuse squamous papillomatosis. In other organs, the causal link between human papillomavirus infection and cervical, anogenital, and some oropharyngeal malignancies has been established by both molecular and epidemiological data. Management Owing to paucity of evidence, it is unclear how to manage this. I guess we can translate knowledge from other areas and use this in oesophagus Isolated small papillomas are easy to ablate with a quick 'zap' of APC. For larger areas of more diffuse papillomatosis, ablative techniques, such as APC ablation or cryoablation or radiofrequency ablation may all be considered. However biopsies or even EMR may be prudent of more 'chunky' areas to rule out possibility of 'prevalent' dysplasia/malignancy. Bjorn has treated a couple of patients with very large areas of oesophageal squamous papillomatosis with APC ablation. Of course, it's quite daunting when you start and it takes a special patient not to freak out when belching up the fumes of vaporised mucosa (a GA would make it easier for the patient of course). However, these lesions actually turn out to be easy to ablate and you will be surprised at the progress when the patient returns for a re-check (usually about 3 months later). However, most patients will probably require 3-4 sessions when the surface area involved is extensive as in this case. Of course, it's difficult to give a general advice about management. Clearly the risk of an elderly patient living long enough to develop a SCC must be small. Conversely, in a young patient, ablation to try to clear the oesophagus will avoid the need for surveillance and is probably justified. Reference Alomari et al Successful Treatment of Extensive oesophageal Squamous Papillomatosis With Cryotherapy, ACG Case Reports Journal: March 2019 - Volume 6 - Issue 3 |
Categories
All
|