|
A 46 year old lady with autoimmune hepatitis is admitted with jaundice, and deteriorating LFT's. She is started on 40mg of prednisolone but has a small haematemesis a couple of days later. On the morning of her endoscopy, nursing staff has documented that she is confused. However, on arrival to the endoscopy unit she is very drowsy. There are no focal neurological signs and the nurse who has escorted her down from the ward denies that she has been given any sedatives. You review her recent blood results:
Hb 125 WCC 12.9 Plat 85 Bili 250 µmol/l AST 310 iu/l ALP 230 iu/l Albumin 33 g/l Bicarbonate 15 mmol/l Blood gases on air pH 7.29 pCO2 2.9 kPa pO2 16.8 kPa Anion gap 25 WHAT WOULD YOU DO NEXT?
■ Check the blood sugar
Absolutely but do you expect the level to be high or low???
■ Check the clotting
Hmm, of little relevance to her drowsiness
■ Check her U&E's
Hard to imagine that it will affect your immediate management?
■ Request a CT head
Would this really be your first intervention?
■ Go ahead with the OGD
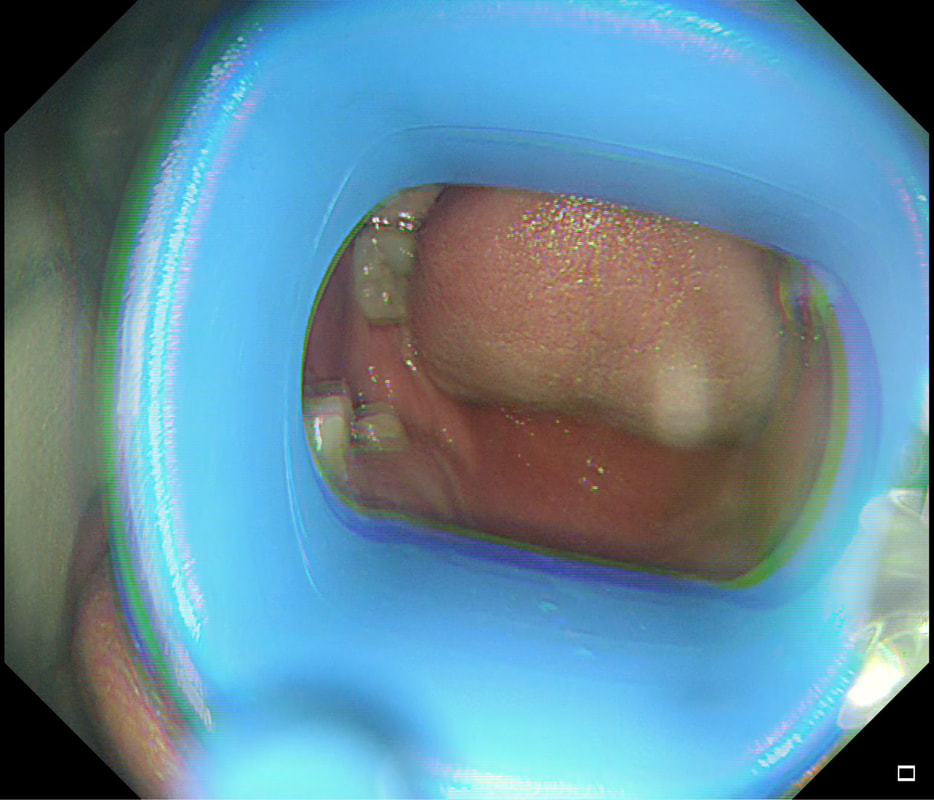
May or may not be 'correct' but wouldnt' you do something else first?
explanation
This is a difficult question as the initial thought is; "What could possibly precipitate coma in a patient with liver disease?
Of course the answer to that questions is:
However, you may have failed to notice that the coma occurred after starting her on high dose prednisolone and that the patient has a marked metabolic acidosis? Next you need to rule out the possibility of 'steroid induced ketoacidosis' by checking the blood glucose level. Of course, a blood sugar is much quicker than getting a head scan and should be done before even considering going ahead with the OGD. Would I then go ahead with the endoscopy? Hmm, yes IF the patient has more solid evidence of a significant UGI bleed with haemodynamic instability and after resuscitation with insulin and fluids etc. |
Categories
All
|