|
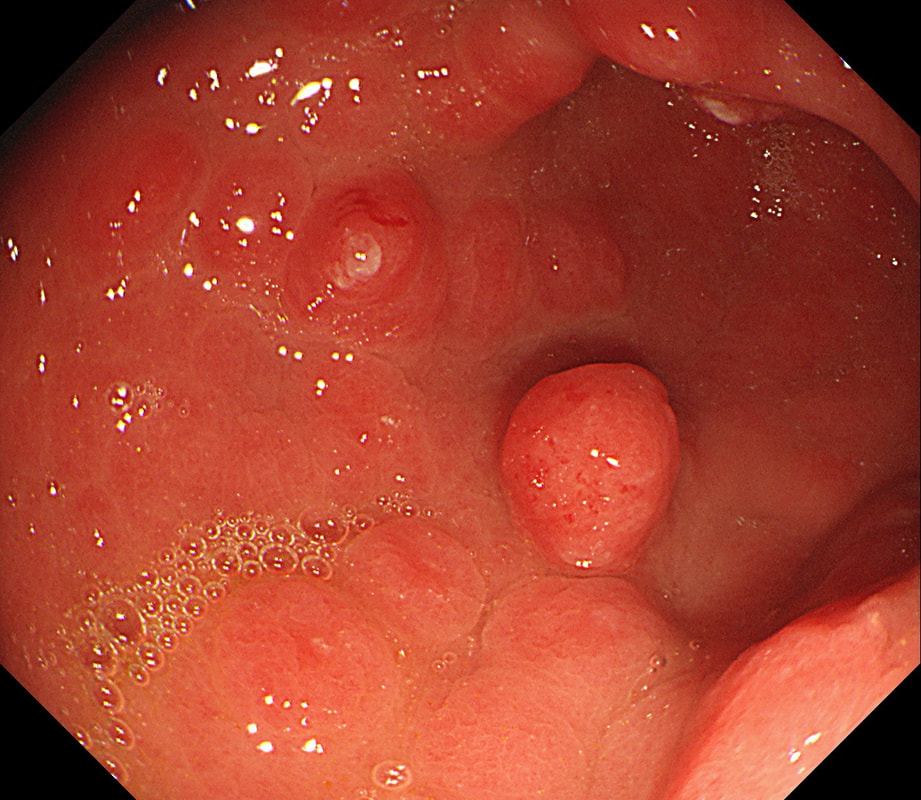
This is an odd looking, almost 'nodular' antral gastritis. You may be surprised that this appearance is typical for a certain type of gastritis ...
WHICH TYPE OF GASTRITIS?
■ Lymphocytic gastritis
Mucosa is usually ulcerated in LyC gastritis
■ Eosinophilic gastritis
You are correct!
■ H.pylori associated gastritis
Can look weird but not classically nodular
■ Collagenous gastritis
Is endoscopically invisible!
■ CMV gastritis
Usually ulcerative
explanation
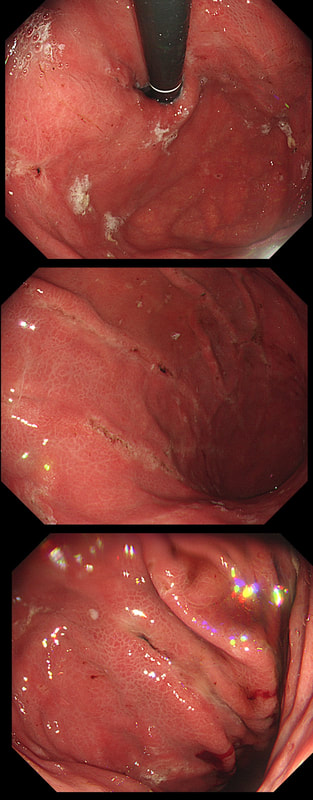
This nodular appearance is typical of an 'eosinophilic gastritis'. In textbooks you also find that lymphocytic gastritis can give rise to this appearance. However, in my experience LyC gastritis is usually intensely red with superficial linear ulceration. See my example below. CMV gastritis look similar but the ulcers are usually round rather than linear.
Anyway, finding more than 30 eosinophils per high power field (HPF) in at least five HPFs has been suggested as diagnostic. There is an argument that pathologists shouldn't make a diagnosis which doesn't change management. Not sure that I agree with this. After all, their job is to describe what they see! Nevertheless, it's probably prudent to ask about food or drug allergies, and consider if patient is atopic. A search for Helicobacters is probably also indicated. I would probably also consider taking further samples from the oesophagus as unrecognised and untreated eosinophilic oesophagitis can ultimately develop into a stricturing disease. Apart from this, it's difficult to know what to make of this diagnosis! Would you do a colonoscopy to chase after the possibility of asymptomatic IBD? |
Categories
All
|