|
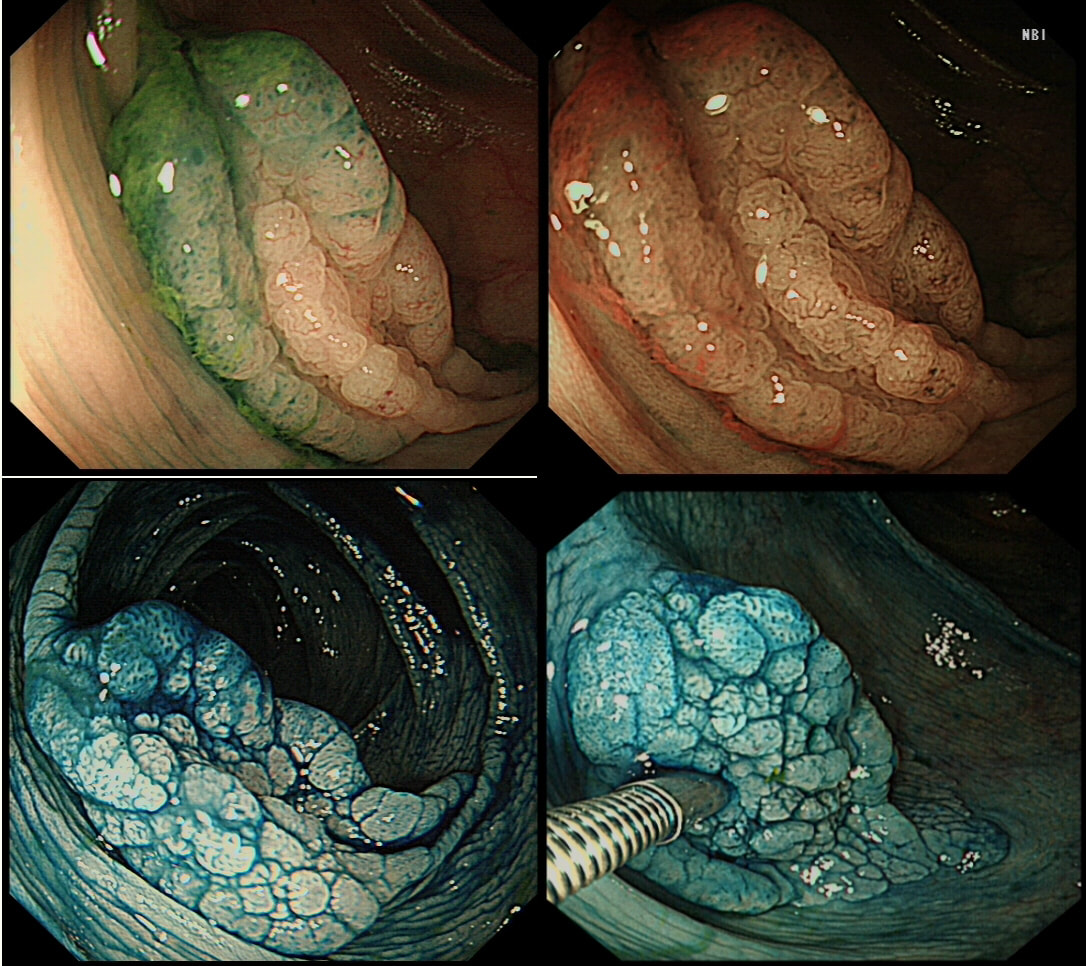
This lesion was found in the ascending colon and was subsequently referred for endoscopic resection.
WHAT IS YOUR ENDOSCOPIC DIAGNOSIS?
SSL
CORRECT!
TUBULAR ADENOMA
INCORRECT!
TUBULO-VILLOUS ADENOMA
INCORRECT!
VILLOUS ADENOMA
INCORRECT!
EXPLANATION
In the indigo carmine dye images, you can see some large, round/oval crypt openings. This was a Sessile Serrated Lesion which actually harboured HGD. 75% of our Facebook group members got the diagnosis right.
The confusing thing is that the growth pattern is that of a LST-G, which of course means that it should be a TVA! I wonder if there is any way I could have predicted the dysplasia? The fact that the lesion is rather "chunky" (but still soft) and not thin and flat, is the sign dysplasia within an SSL . The image caused some controversy back in 2014. Several endoscopists didn't believe that an endoscopic diagnosis could be made. In fact, some hinted that it would be inappropriate to second guess histology. After all, these are the guys with all the answers right? You should stand 'cap in hand' and wait patiently until they tell us what we have seen. It makes my blood boil ! Fortunately, endoscopy has moved on from those dark times. Now we recognise that we have a duty as endoscopists to contribute to the diagnosis. The diagnosis is based on an assessment of the entire lesion and it's degree of lifting. In contrast, our poor pathologists can only give an opinion on the square mm of tissue which we provide them with. That is why they need microscopes! By recognising our responsibility, we accept a duty to develop expertise. Of course, this directly benefits patients as we are more likely than our pathologist to recognise an early malignant polyp and thus target samples to the area which is the most suspicious in appearance. Our pathologists also benefit from our diagnosis, although some endoscopists believe that we shouldn't tell them anything as it could bias their assessment ☺ . To conclude, the combined endoscopic and histological assessment is what is most likely to reach the correct diagnosis - a Team Effort !!! |
Categories
All
|