|
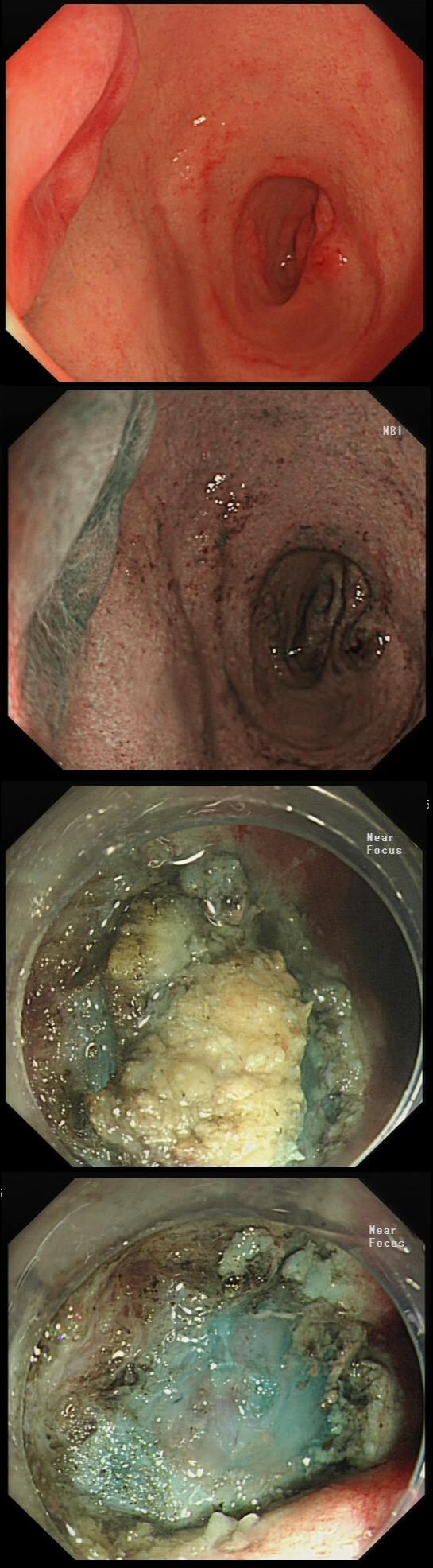
This lesion was referred for resection just beyond the pyloric ring. It seemed to lift well but rather to my surprise, the snare cut through the base of the lesion (bottom image on the left). It took some further lift and a stiff snare to scrape the lesion of the muscle propria layer.
WHAT IS THE LIKELY HISTOLOGY?
■ Adenoma
Adenomas are usually not umbilicated ...
■ Brunners gland hyperplasia
I don't bother to remove those and they are not umbilicated!
■ Gastric heterotopia
Is usually found at this location but never require EMR
■ NET
Of course it is - it's umbilicated !!!
■ Early malignancy
Would be VERY rare in the duodenal cap!
explanation
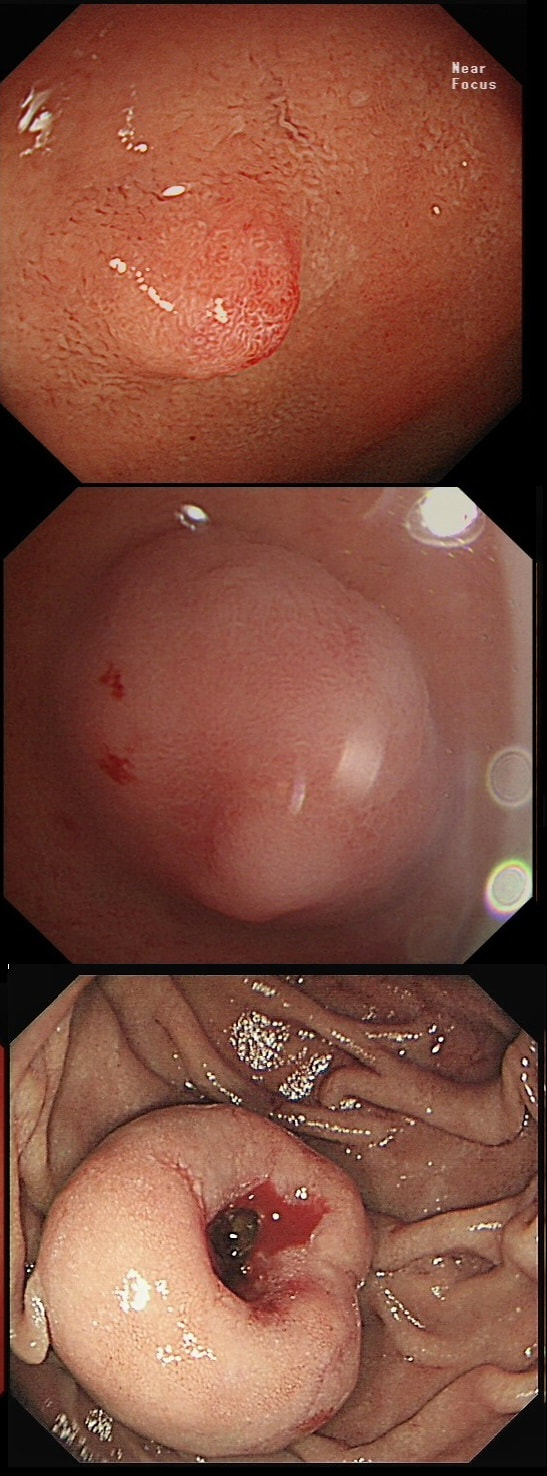
The lesion is umbilicated... As you probably remember, umbilicated lesions in the duodenum are usually NET's. For some reason, they look different to NET's found elsewhere in the gut, where thin vessels are usually seen crawling up their sides. In the photograph below, you can see that at the very earliest stage (first image), there is no central indentation. However, very soon a subtle central dip develops (second image) which at the advanced stage (when I was tasked with removing the lesion), it has a deep central pit which was intermittently bleeding.
This proved to be a WHO grade I NET (neuroendocrine tumour, with a mitotic rate <2%). These lesions always seem to be tethered down close to the muscle propria and can be difficult to remove without taking a chunk of muscle propria with it. Duodenal NET's should of course be discussed at the 'neuroendocrine MDT' and usually end up having: 1) Measurement of plasma chromogranin A (pCgA) levels. CgA is produced by all cells derived from the neural crest and high levels are found particularly in patients with metastatic disease. 2) A ‘gut hormone screen’ (measurement of gastrin, glucagon, vasointestinal peptide, somatostatin and pancreatic polypeptide levels). 3) Finally, an ‘octreotide scan’ (somatostatin receptor scintigraphy) or, even better, a PET/CT scan using peptides that bind to somatostatin receptors (68Gallium-DOTA-TOC/NOC/TATE). |
Categories
All
|