|
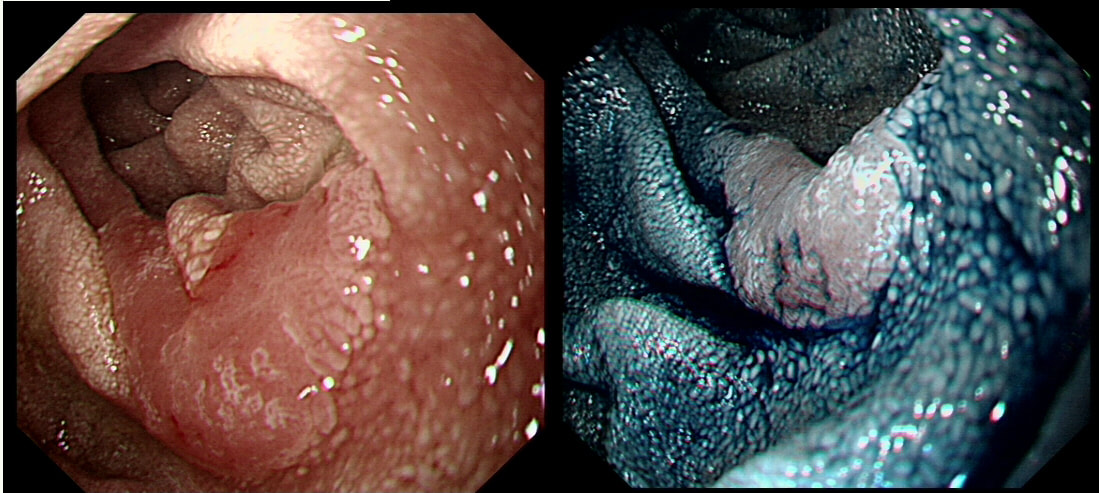
This polyp was found in the duodenum of a 65 yr old man undergoing OGD for dyspepsia.
WHAT IS YOUR DIAGNOSIS?
a) Hyperplastic Polyp
INCORRECT!
b) Lipoma
INCORRECT!
c) Neuro-Endocrine Tumour (NET)
INCORRECT!
d) Adenoma
CORRECT!
e) Carcinoma
INCORRECT!
explanation
>95% of our facebook group correctly recognised that this lesion is a sporadic duodenal adenoma. Of course, you should now consider offering your patient a colonoscopy as there is a link with colorectal adenomas.
Actually, it turned out to be tubular adenoma with low-grade dysplasia (TA+LGD). The risk of malignant conversion in a 'sporadic duodenal polyp', is probably very low. Nevertheless, I do remove these lesions in patients who are at least "reasonable fit" with a life expectancy of at least 10 yrs. Because there is a 1:20-30 risk of late bleeding even after removing a small polyp, I always apply clips to the mucosal defect. In addition, I tend to reject patients who I think may not 'cope well' with a 2 unit blood loss or an emergency laparotomy. By the way, I think that using a banding device such as the Cook 'Duette' or the Boston Sci 'captivator', is probably dangerous in the thin walled duodenum. You should also be careful with the use of the haemostatic forceps. There is a real risk of a late perforation if too much heat is applied to the thin mucosa. Finally, immediate perforations are often difficult to recognise in the duodenum. Not sure why this is but my last perforation was pinhole and entirely invisible at the time of the procedure. I know this because I watched the video clip several times afterwards. After a few hours exposure to pancreatic juice, the hole was an a centimetre in diameter (measured at the time of laparotomy) and the poor patient spent another 2 months in hospital recovering. Fortunately, 12 months later the external drains could be removed. A recent study published in GIE [Fukuhara S et al. Management of perforation related to endoscopic submucosal dissection for superficial duodenal epithelial tumors. Gastrointestinal Endoscopy 2020;91(5):1129-11370] reinforced my view. This Japanese multicentre study reported on the management of perforations following ESD resections of duodenal polyps. A perforation complicated 14% of ESD resections and only 1/3 of perforations could be closed completely endoscopically. Fortunately, even perforations which were not completely closed, only 2/36 perforations required surgery. The remainder could be managed with the placement of an 'endoscopic naso-biliary and pancreatic duct drainage tube. The duodenum is "Tiger Country" and I recommend that you avoid polypectomy here unless you have full 24 hour/364 days/year backup by expert upper GI radiology and specialist surgical backup. You need the reassurance that it will be a friendly and support specialist upper GI surgeon who is sorting out your patients biliary peritonitis at 3 O'clock in the morning! |
Categories
All
|