|
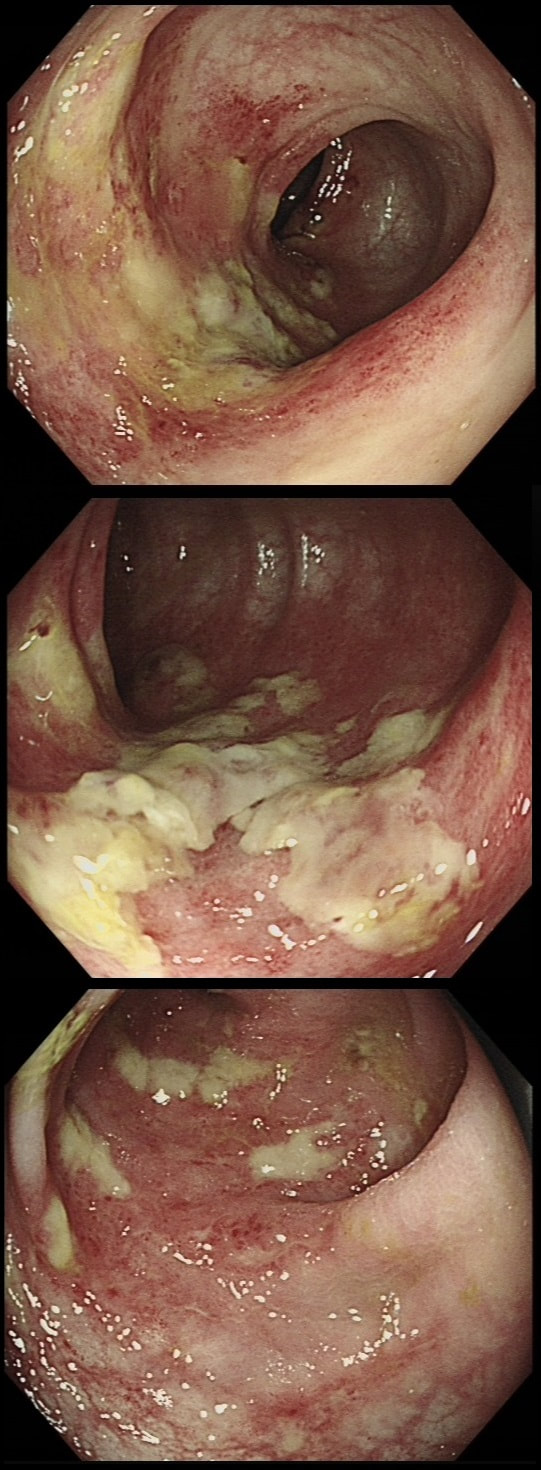
This 70 year old patient with known ischaemic heart disease presents with sudden onset bloody diarrhoea. He undergoes a flexible sigmoidoscopy the following morning and this is what the sigmoid colon looks like. With support and conservative measures symptoms subside and the patient is discharged a week later. However, a week later the patient presents again. Now with hypotension, abdominal distention, fever and a raised white count. An abdominal X-ray is done on admission (below).
WHAT IS THE LIKELY DIAGNOSIS?
■ Colonic stricture
Too soon for this!
■ Another attack of ischaemic colitis
Unfortunately, yes!
■ Pseudomembranous colitis
He didn't actually receive any antibiotics last admission
■ Crohn's disease
Unlikely !
explanation
There is little mystery that the first presentation was due to ischaemic colitis. The second presentation is more tricky. He actually presented with an ileus and pain this time. Actually, the patient had been on aspirin but this had been stopped at the previous admission. This was clearly a mistake as the second presentation turned out also to be due to ischaemic colitis. This time the ischaemic colitis was more severe but he did recover in the end.
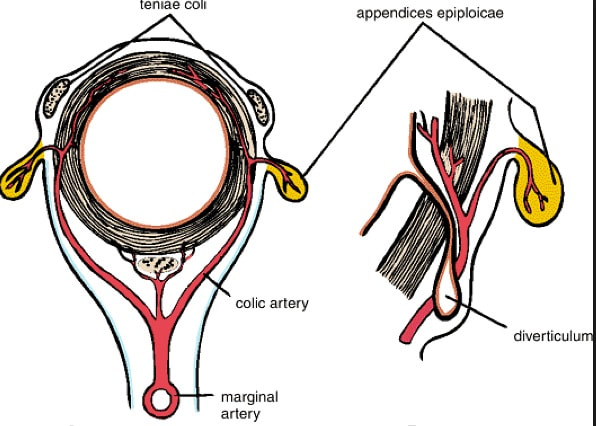
After ischaemic colitis about 10% of patients develop and ischaemic stricture but it takes longer than a single week to develop. The hallmark of an ischaemic colitis are areas of longitudinal ulceration, on the anti-mesenteric border (90° to any diverticulum) where the blood flow is the slowest. Of course, endoscopically its difficult to tell where the omental reflection is situated. However, the ulceration will run along one aspect of the colonic circumference. Of course in the epicentre of the ischaemic (typically around the splenic flexure), the ulceration may well be circumferential. Ischaemic colitis is surprisingly easy to confirm histologically as the pathologists look for crypt withering and fibrosis. By the way, if the mucosa looks dusky and there is no bleeding on taking samples, the likelihood is that the colon is turning gangrenous, associated with a >50% mortality rate. |
Categories
All
|