|
These polyps were found in the stomach of a 40 year old man on a Barrett's surveillance programme WHAT WOULD YOU ADVICE?
■ We should eradicate your Hp
This patient is VERY unlikely to have H.pylori
■ We should remove these endoscopically
An unnecessary job unless one look wonky, like perhaps that single red one!
■ We should stop you PPI
But the patient has Barrett's ?!
■ We should stop you PPI
That's what I would do !
explanation
Of course, this is a Fundic Gland Polyps/Cystic Gland Polyps . They are usually multiple, somewhat transparent sessile polyps, usually in the 1-5mm in diameter and located in the body and fundus.
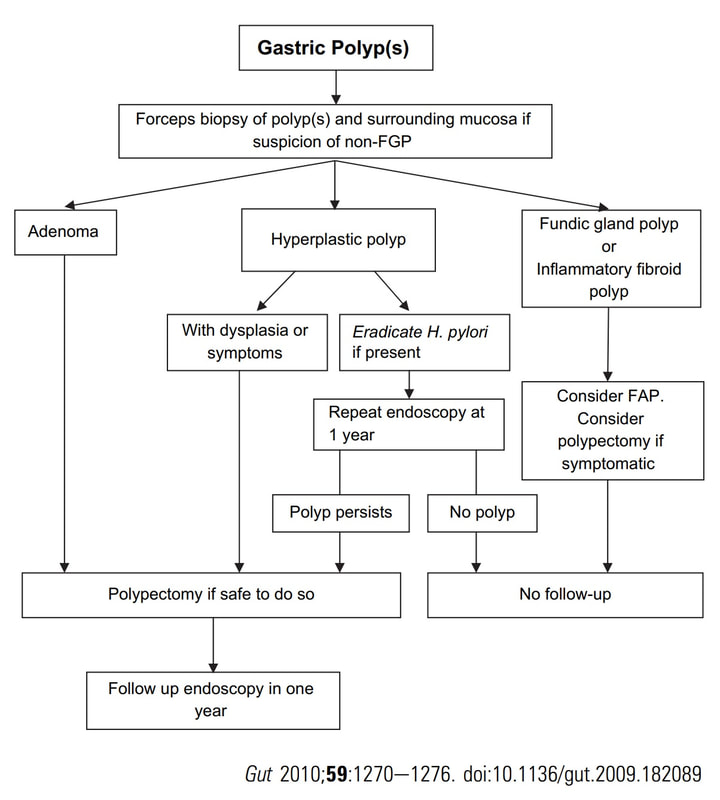
Histologically there are cystically dilated glands lined by gastric body type mucosa. Of course, there is no need to sample these. A study patients with FGPs reported that they can be diagnosed with a high degree of accuracy based on endoscopic appearance alone (J Clin Gastroenterol 2003;36:399-402). The sporadic polyps are caused by activating mutations of the beta-catenin gene. Not sure how an APC gene mutation (you may remember are involved in FAP), could give rise to FGP’s though! Furthermore, I don't know how the use of PPI's can be linked to the development of FGP's. Presumably its something to do with the prolonged hypergastrinaemia and enterochromaffin cell-like (ECL) hyperplasia? I have seen a couple of cases of cancer developing within a FGP. In both cases the patient had FAP and the polyps were markedly larger than all the surrounding cystic fundic polyps. There have been case reports of dysplasia arising within sporadic fundic gland polyps. A few series have reported a <1% risk of sporadic FGPs harbouring dysplasia (Am J Surg Pathol 1998;22:293-298, Eur J Gastroenterol Hepatol 2003;15:1153-6, Endoscopy 1995;27;32-37). I must admit that I don't believe the figure of <1% risk of dysplasia in a sporadic FGP. I suspect that these series consist of rather selected cases. Of course by only selecting polyps 10mm or larger, you would be filtering away 99% of the FGP's, leaving only the 'far above average risk lesions' behind. Nevertheless, the BSG recommend sampling some of them to confirm the diagnosis but not to set out on any attempt to remove them. Of course, this advice is different to the advice for Hyperplastic polyps which ARE usually linked with H.pylori and also a greater risk of developing cancer. The BSG advice is summarised in the algorithm below. Sporadic FGPs are not associated with either H.pylori gastritis or atrophic gastritis. In fact, it has been proposed that H. pylori infection may have an inhibitory effect on the development of FGPs. Of course, you wouldn't stop the PPI in a patient with Barrett's. Actually there is no evidence that patients with unstable Barrett's are any more or less likely to progress to cancer if they stop their PPI. However, there must be a point (I presume) when the use of PPI is beneficial in the 'evolution' of Barrett's. Are patients on a PPI less likely to develop Barrett's or to develop damage the stem cell DNA? Not sure! The BSG do recommend a colonoscopy in patients below the age of 40 yrs. to rule out the possiblity of FAP. However, as the average age of colorectal cancer in patients with 'attenuated FAP' is 55 yrs, I would personally recommend a colonoscopy in patients above the age of 40 yrs. |
Categories
All
|