|
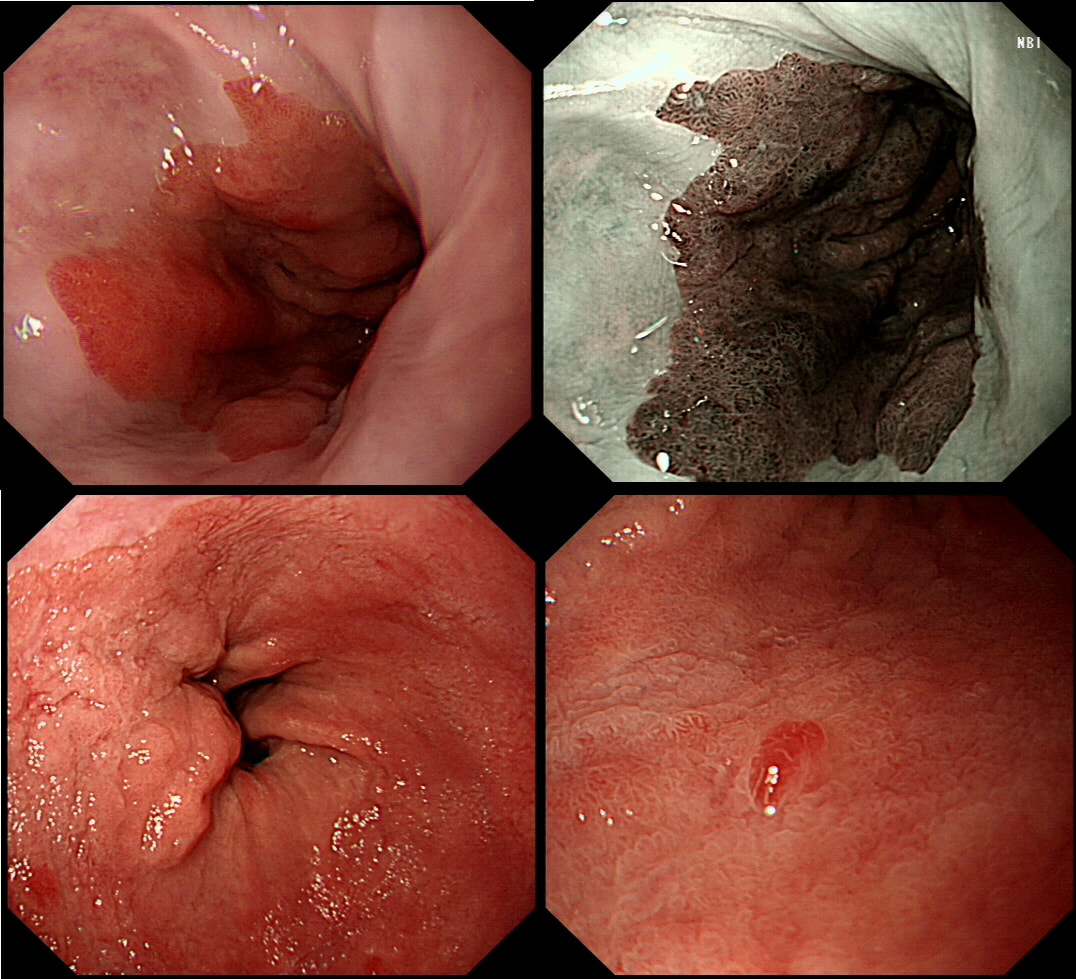
This pt with short stretch of Barrett's have previously had dysplasia detected within his Barrett's. He is now attending a follow up gastroscopy for consideration of RFA.
WHAT WOULD YOU DO NEXT?
■ TAKE ANOTHER SET OF SAMPLES
NOT INCORRECT☺!
■ GO AHEAD AND RFA
INCORRECT!
■ DO AN EMR FIRST
CORRECT!
EXPLANATION
On Facebook, most (69%) suggested that the nodule needed to be removed first. However, first taking another set of samples, isn't 'wrong'. Provided of course that you also sample that suspicious nodule at 6 O'clock (bottom right photograph)!
I actually removed that nodule at the 'index examination'. As expected, it was confirmed as harbouring IMca. Not a surprise as 'Nodules are NEVER allowed within Barrett's. At the same time, I also obtained a set of samples from the more unremarkable surrounding Barrett's. This revealed a mixture of high and low grade dysplasia (i.e. HGD and LGD). A few months later the patient returned for his RFA. By the way, unstable Barrett's often has a subtly irregular surface, slightly more red than usual and often with patches of superficial ulceration. In particular, superficial ulceration almost certainly means that the Barrett's is dysplastic. Presumably this is because the 'Goblet cells' are the first to disappear when the Barrett's become unstable. Of course, there is no hurry to offer patients RFA. I do take my time, first having a chat with the patient about the 'issues' of; pain afterwards (a prescription of 'oxetecaine & antacid' helps), the need for continued surveillance ('because the cure will not last') and reassure that continued 6-monthly surveillance is no less effective than RFA in reducing their likelihood of dying from Barrett's cancer. What I don't mention is that most patients on Barrett's surveillance die from cardiovascular disease. Of course their risk of dying from oesophageal cancer may well be below the average population risk. Hmm, isn't it odd that we never see this benchmark figure of 'average population risk' in publications? Arguably, it's the ONLY benchmark that matters !!! |
Categories
All
|