|
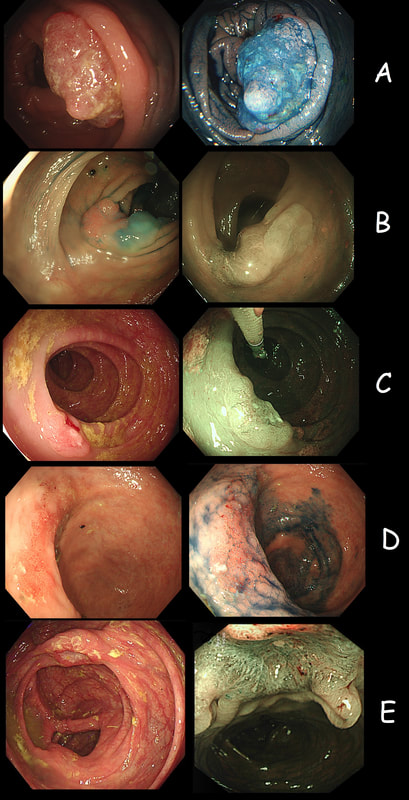
As you know, colonoscopy protects less well against future cancer in the right hemi-colon, than cancer elsewhere in the colorectum. Here are 5 lesions, all found in AC. Four are malignant and one isn't ...
WHICH ONE IS NOT A CANCER?
■ A
SM3 invading CRC with very little adenomatous tissue present
■ B
Cancer arising in an SSL !
■ C
A very superficial CRC removed by ESD
■ D
Yes! This is a 'caecal patch' in UC
■ E
Nope, its a mucinous carcinoma!
explanation
You can probably tell that the first lesion is a cancer because of it's nobbly surface and lack of crypt pattern in places. It was a sm1 invasion T1,N0 cancer (i.e. invading up to the muscularis propria layer but didn't invade into it).
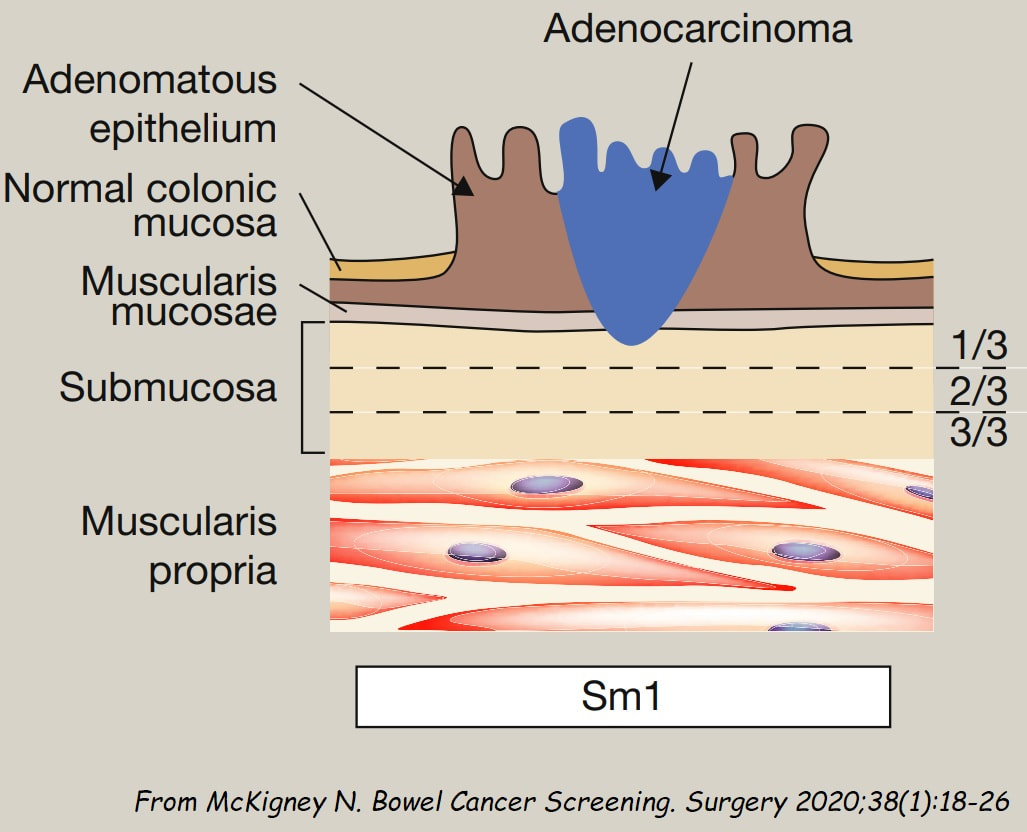
The second lesion is a sessile serrated lesion with a small cancer at it's edge. The staging was identical to the first lesion (sm1 invasion T1,N0 cancer). The third lesion was a superficial carcinoma (sm1 invasion only) and the only in the series actually removed endoscopically. The fourth lesion is the 'odd one out'. It's actually a 'caecal patch' in a patient with ulcerative colitis, only affecting the rectum. The final lesion was a 'mucinous adenocarcinoma'. Interestingly, analysis of the initial biopsies reported 'TA+LGD'. Don't believe everything those pathologists tell you! Your eyes don't lie! There is a further interesting twist here. After another set of samples, got the pathologists to agree with our endoscopic diagnosis, we were surprised that the patient was turned down for surgery due to severe comorbidities. Rather begs the question what was the point in putting the 85 year old gentleman through two colonoscopies !!! Anyway, that was 4 years ago and he has still not developed any symptoms from his cancer!? A recent CT confirmed that it was slowly growing and was now annular but without any evidence of spread or obstruction. Interesting and clearly turning someone down for surgery is not necessarily a 'bad thing' ! Still leaves me wondering why they keep scanning the poor bloke though? Below I've attached a reminder about the 'Kikuchi staging' which your pathologists should use to stage superficial flat cancers. |
Categories
All
|