|
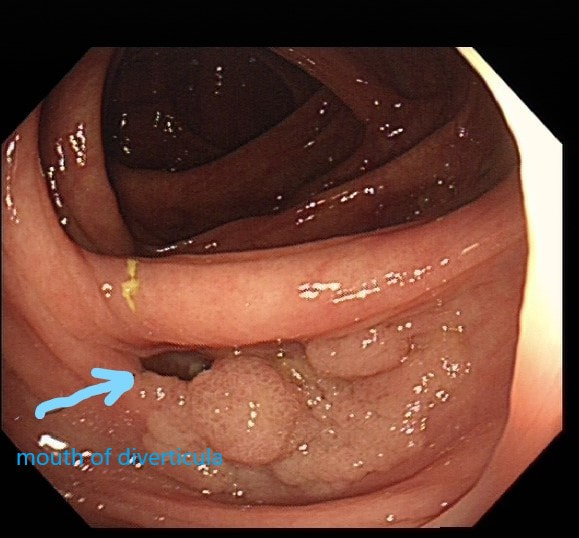
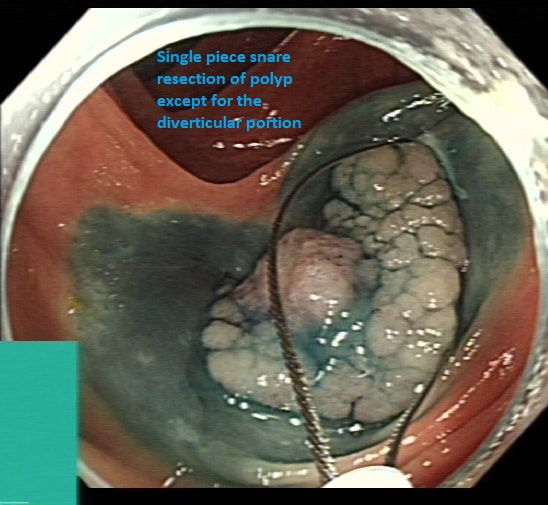
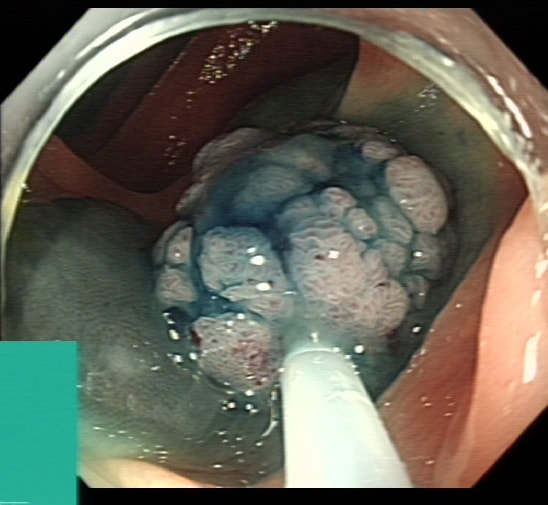
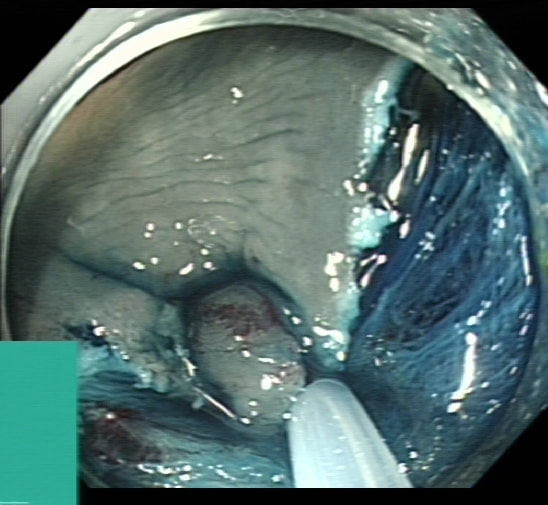
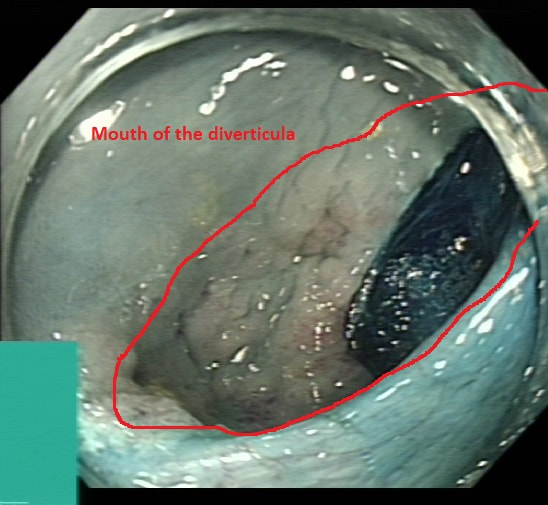
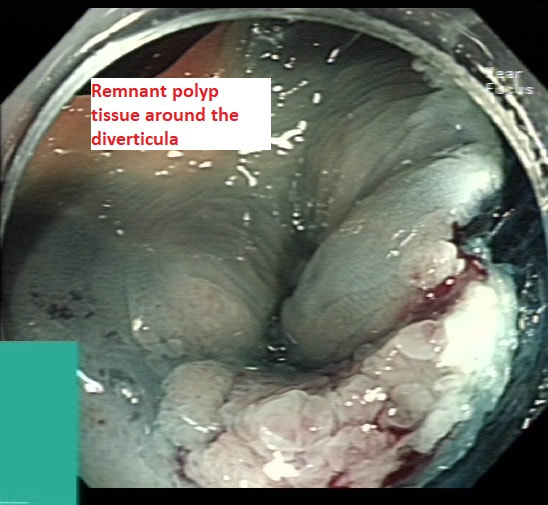
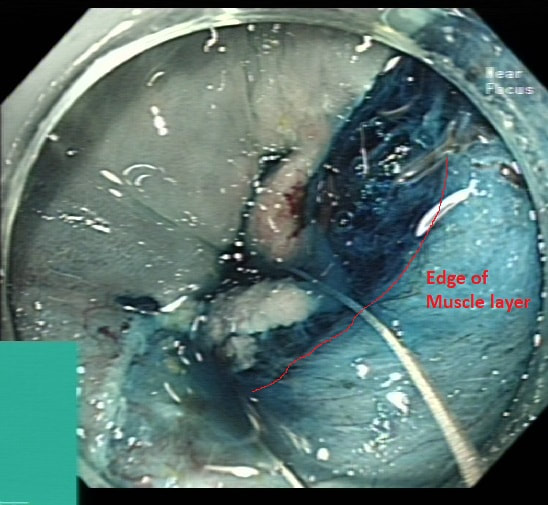
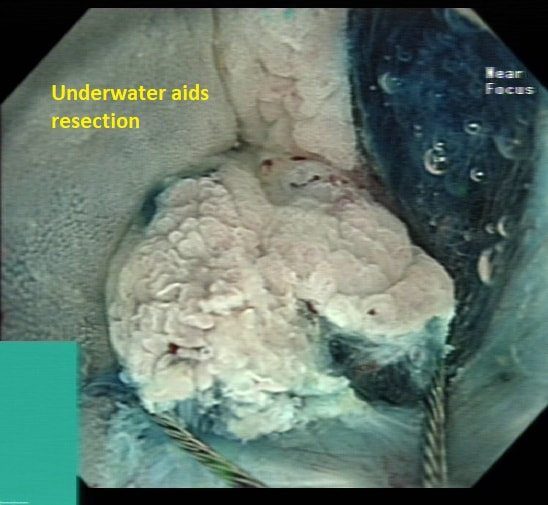
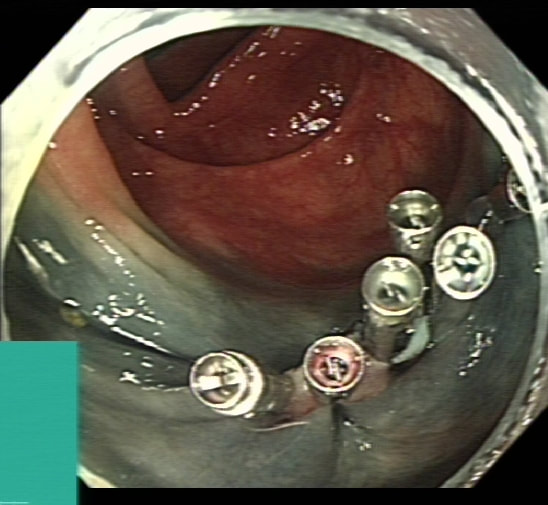
Posted by Dr Pradeep Mundre Highlighting some key points, Tips/Tricks when considering endoscopic resection of polyps invading diverticula 1. More often the polyp just invades partially superficially into the diverticula, making it easy to tease it out during endoscopic resection 2. For most such polyps conventional EMR should be enough- Ensure that the lifting is in the right plane starting lift away from diverticula gradually moving towards. 3. There is a risk of perforation as no muscularis propria in diverticula 4. Clear cap always helps for any complex resection 5. There is often poor lifting of polyp around the diverticula 6. When resecting the polyp tissue within the diverticula, deflating the lumen and releasing the luminal tension helps 7. Stiff snare (I used medworks flat band snare here) may help get better hold of polyp 8. Underwater resection helps similarly 9. Despite macroscopically complete resection, risk of Recurrent/Residual polyp is high, so always consider site check @ 4-6 month and once again at 18 months 10. Other methods include EFTR, Band ligate and leave (post biopsy) approach or surgery Dr Pradeep Mundre
0 Comments
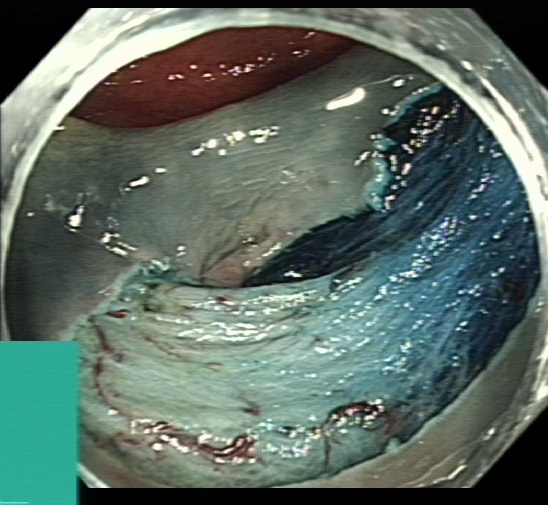
Short video of use of traction wire - Medtronic ProdiGI use in a ESD of a hepatic flexure LST NG type leaning towards pseudodepressed type , but can argue its flat type
Few points about LST NG Pseudodepressed type
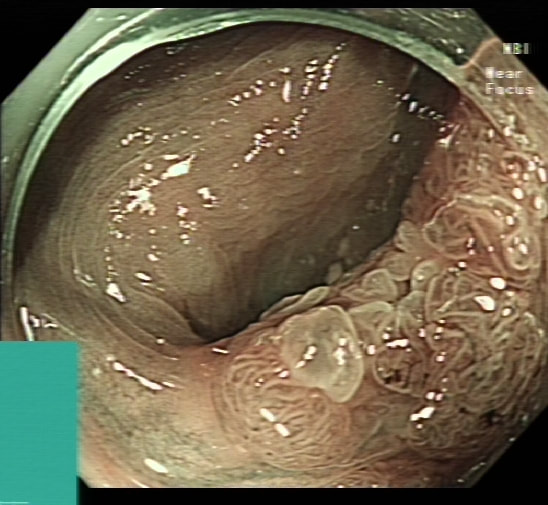
This is a 'difficult polyp because it's almost impossible to get any closer than this. It's arising from a fold in the ascending colon, just downstream to the caecum. Keep an eye on that scopeguide image and you see why it's so difficult.
Of course this makes it difficult to tell how far the polyp extends into the caecal sac. Fortunately, I was able to get glimpses of just behind the lesion which told me that it didn't extend far beyond the fold. Had this lesion extended into the 'valley' behind that fold from which its arising, it would have been a 'show stopper' to me. Another reason to 'attack' is that the lesion does look benign with a reassuring gyrate crypt pattern of a TVA. Naturally, any polyp of this size will have a 15% risk of actually containing an unexpected focus of cancer within. Because our therapeutic waiting list is in mess in the aftermath of Covid, I do encourage everyone to sample the sessile lesion even though you are planning to refer it for resection. Such sampling on the surface of large sessile lesions doesn't induce any fibrosis and provides 'some' (very limited of course) reassurance that the lesion isn't malignant. The main teaching points in the video are:
 Of course, its important to carefully examine the entire stomach especially in premalignant stomach for any synchronous lesions despite seeing something very evident. The above video is follow up Endoscopy 3 months after the removal of the large sessile lesion in the antrum (photo). The polyp was removed by ESD and histology confirmed a Villous adenoma with low and high grade dysplasia as well as a small focus of adenocarcinoma – pT1aM2 (clear margins). Wisely, it turned out, the patient was recalled for early 'site-check' and examination of the rest of the stomach. This turned out to be worth while ! WHAT DO YOU THINK THE LESION IN THE VIDEO IS? explanation
It is very easy to overlook synchronous lesions when there is a large 'eye-catching' lesion, drawing all your attention. My learning point is that its important to look for synchronous and eventually metachronous lesions and not to get blinkered by the obvious pathology! Patients do sometimes have dual pathology ! Yes, it happens !!! Actually, the second lesion was confirmed to be an Intramucosal adenocarcinoma - moderately differentiated pT1aM3, with no lymphovascular invasion and clear lateral and deep resection margins . This was a 'curative resection' as per BSG Guidelines for endoscopic resection as the risk of nodal metastasis in such leisons is probably <1%. Some bullet points on Synchronous tumours (Dysplasia or cancer)
And some on the topic of Metachronous tumours
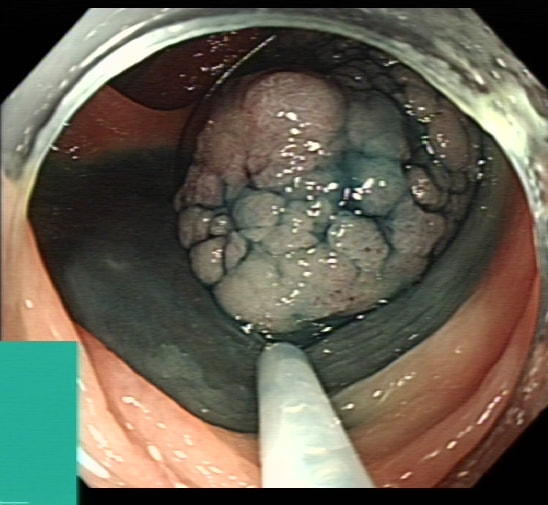
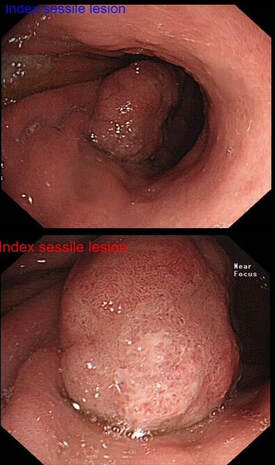
Reference Banks M, Graham D, Jansen M, et al British Society of Gastroenterology guidelines on the diagnosis and management of patients at risk of gastric adenocarcinoma. Gut 2019;68:1545-1575. A 60 year old woman with type 2 diabetes and hypertension was found to be FIT+ve under the UK Bowel Cancer Screening Programme. The index colonoscopy, performed by a colleague 2 weeks ago, showed 4 polyps in the sigmoid / rectosigmoid colon. The three smaller polyps (6-15mm diameter) were removed (tubular adenoma, low grade dysplasia). The largest polyp, a 5cm LST-G on a fold at the rectosigmoid junction was left behind for another day. The LST-G was not biopsied. The patient now attends for a further procedure to remove the LST-G (see video…).
The video highlights several tips:
'Rembacken's Resection Rules' is a 'tongue in cheek' list of General Principles which helps me in my endoscopic practise. They have stood the test of time !!!
Sigmoid snare polypectomy in spastic, tight sigmoid. Teaching points include:
Small polyp on thick stalk for snare polypectomy at the recto-sigmoid junction cocked up! Teaching points include:
EMR of a 20mm sigmoid polyp. Main teaching points includes:
A short clip of Lugol's dye spray. Teaching points includes:
|