|
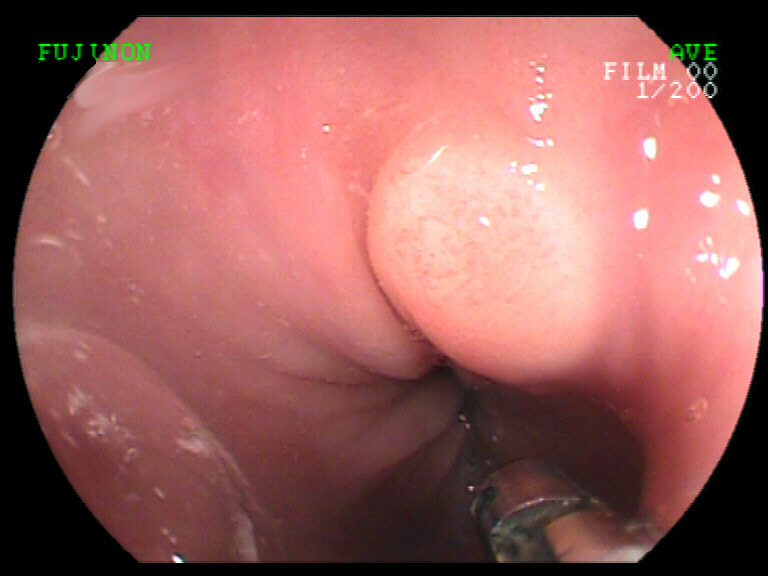
This small lesion was found in the distal oesophagus just above the squamo-columnar junction
WHAT IS THE LIKELY DIAGNOSIS?
■ GRANULAR CELL TUMOUR
CORRECT!
■ LEIOMYOMA
INCORRECT
■ GIST
INCORRECT!
■ NET
INCORRECT!
■ EARLY SCC
INCORRECT!
EXPLANATION
This is the typical appearance of a granular cell tumour (Abrikossoff’s tumour) first described in 1926 by Abrikossoff, a Russian pathologist. These lesions can probably develop anywhere but is mainly found in the skin, mouth and GI tract.
Within the GI tract, the oesophagus is the most common location. Lesions are occasionally multiple (about 10% of cases). Granular cell tumours are said to be more common in women and black people. Superficial biopsies may occasionally fail to confirm the diagnosis as these nodules are submucosal. The differential diagnosis is that of a small lipoma, NET or a leiomyoma (which are much more common in the oesophagus than in the stomach). When detected these lesions are usually referred for endoscopic resection. Unfortunately, as the lesions arise from the deep submucosa, the risk of a local recurrence is high (30-40%). For this reason I now treat the raw EMR surface, immediately post-resection with APC set at low power (30W). By the way, a small proportion of these lesions (<2%) are said to be malignant overall. However, the published literature is confusing as GI and non-GI lesions are frequently combined. Perhaps the only compelling reason for removing these from the oesophagus, is that it is cheaper than surveillance! |
Categories
All
|