|
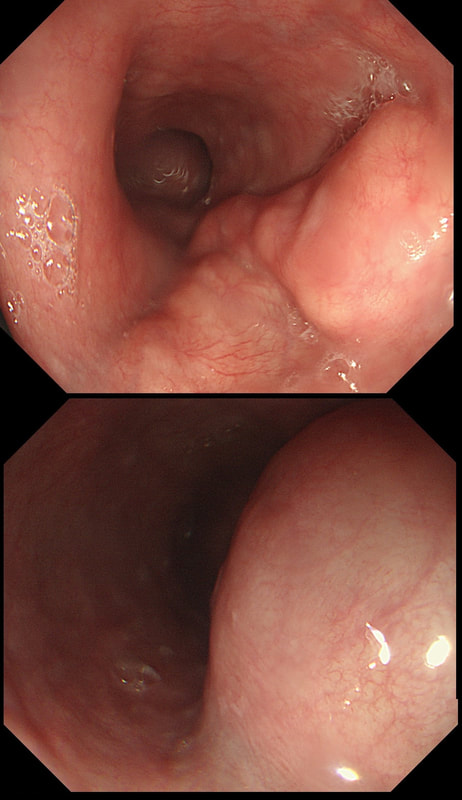
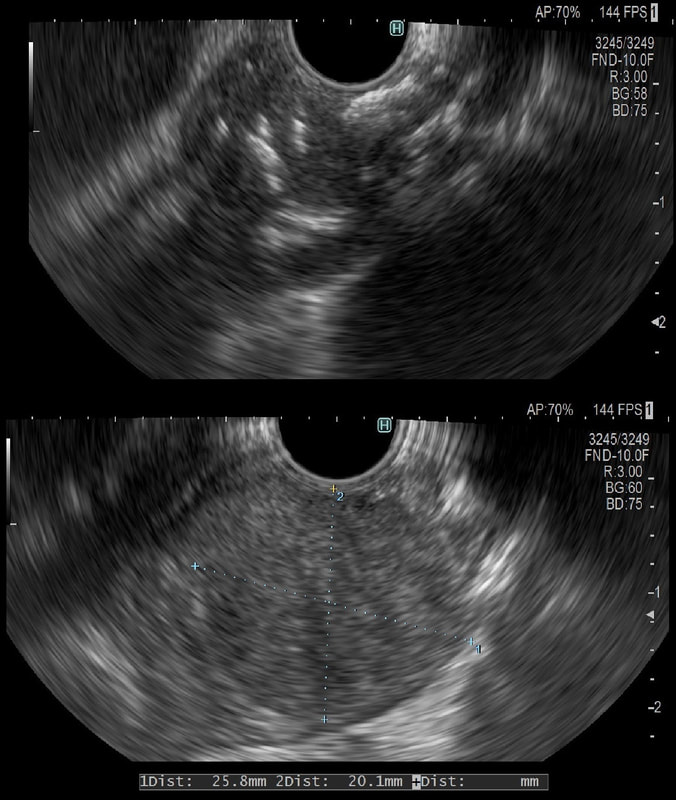
This was an incidental finding in the mid-oesophagus. Subsequently an EUS is organised and the lesion is ultimately removed (histology in the last image)
WHAT IS THE DIAGNOSIS?
■ Neuroendocrine tumour
I've never actually seen an oesophageal NET
■ Granular cell tumour
But it isn't a small white submucosal disc?!
■ Leiomyoma
A shrewd guess!
■ GIST
These are VERY rare in the oesophagus (but common in stomach)
■ Melanoma
Usually look brownish endoscopically!
explanation
Leiomyomas are the most common submucosal lesion found in the oesophagus. No idea why they are so rare in the stomach, where GIST's are the most common submucosal lesion. Correspondingly GIST's are very rare in the oesophagus.
These usually arise from the circular muscle propria layer. On CT they are often calcified and there are of course no nearby nodes to suggest malignant disease. Indeed, malignant transformation is extremely rare and for this reason many centres would ignore a small submucosal lesion such as this, when found in an elderly person. Larger (around 5cm usually) and symptomatic lesions (which are more likely to be leiomyosarcomas) are enucleated surgically. "- They shell out like peas" according to one of our UGI surgeons. However, our local surgeons are also careful to point out that resection usually result in some damage to the muscle propria layer, which require repair as otherwise a diverticulum may develop. With endoscopists spending more time in the 'third oesophageal space' (i.e. the submucosal space), doing ESD's and POEM, the suggestion that we should also remove leiomyomas endoscopically has arisen. May seem like a good idea but I would advocate caution for the simple reason that endoscopically, we are unable to repair the defect we cause in the muscle propria layer ... Oh, how about that 'SMA stain' used in the histology. This is 'Smooth Muscle Actin' stain which does exactly what it says on the tin ...
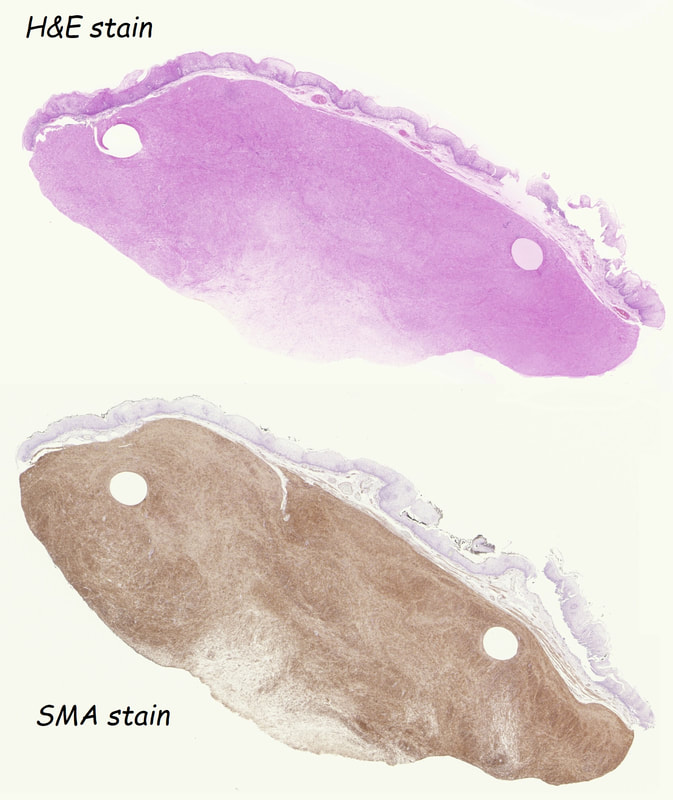
This 25 year old man presented with an attack of jaundice. Here are photographs of his duodenal ampulla and EUS
WHAT IS THE DIAGNOSIS?
■ Impacted gallstone
There is more than just a bulging ampulla
■ Pancreas divisum
Nope!
■ Mass in the head of pancreas
But 'mass' seems to be extending below ampulla
■ Choledochal cyst
Of course, you do ERCP's clearly!
■ Duodenal varices
Looks a little vascular and would be soft to touch!
explanation
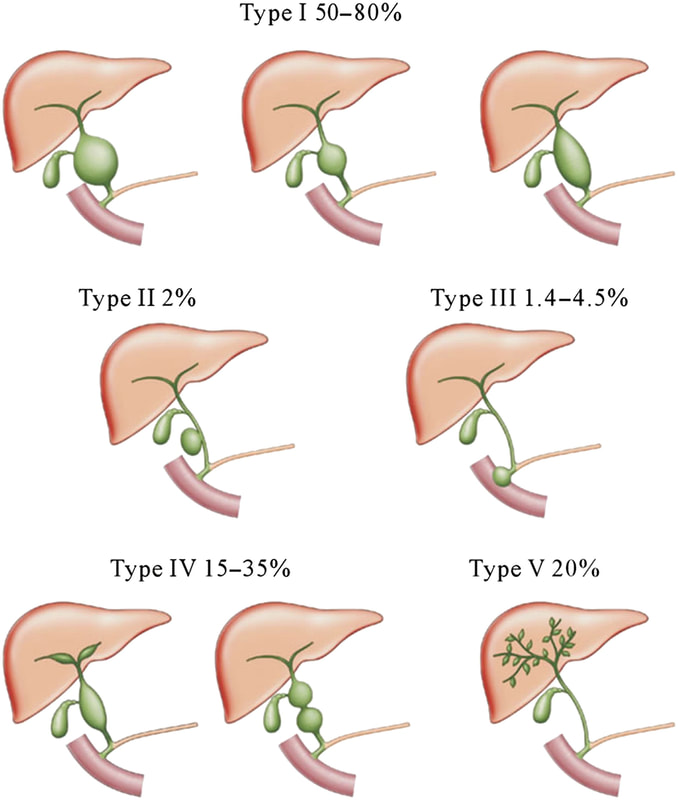
That EUS does confirm a cystic dilatation of the distal part of the common bile duct. Of course, the patient has a 'choledochal cyst' ! These are congenital cystic dilatations of parts of the biliary tree. In this case, only the distal CBD was involved, making this a 'type III' choledochal cyst which is located at the ampulla (see figure below).
Most cases presents as jaundice or pain in infants. Chronic cholestasis may present later with biliary cirrhosis or cholangiocarcinoma. Fortunately, this case was discovered before cirrhosis and the patient was treated with surgery.
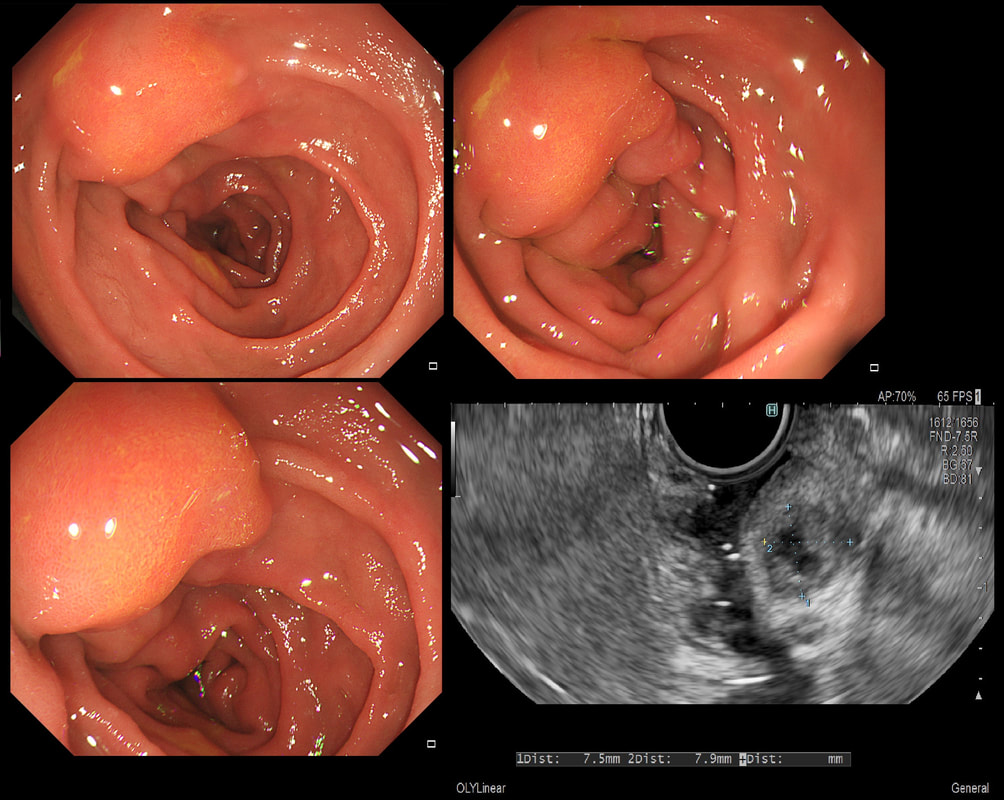
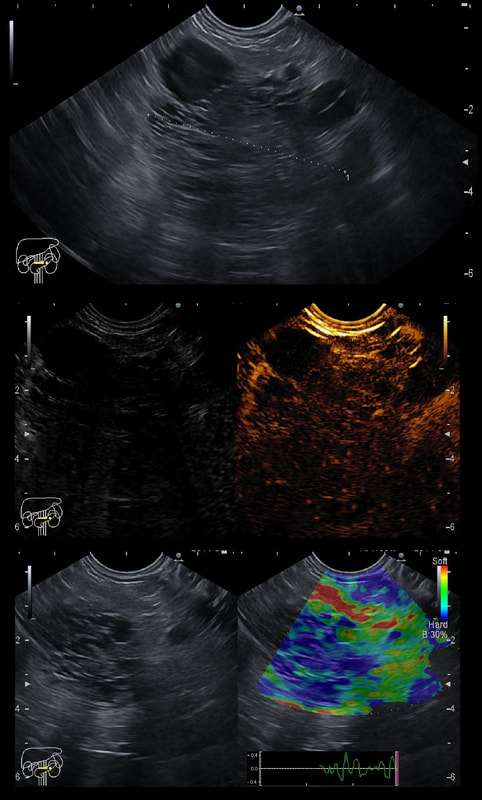
This is an contrast enhanced EUS of a 5cm pancreatic mass together with the doppler (arterial and venous phases) and elastography images
WHAT IS THE MOST LIKELY DIAGNOSIS?
■ Serous cystic neoplasm
Absolutely right !!!
■ Ductal adenocarcinoma
Nope !
■ Neuroendocrine tumor
No again!
explanation
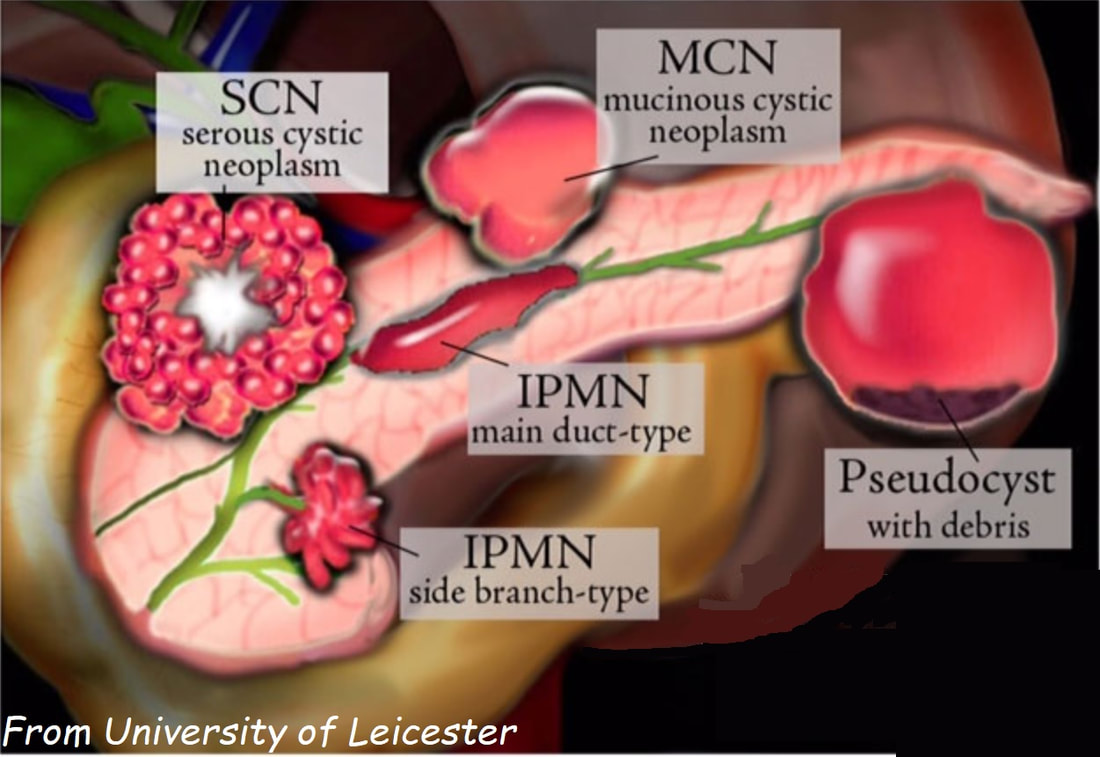
This the typical appearance of a serous cystic neoplasm (formerly called serous cystic adenomas) situated in the tail of the pancreas. The natural history of these lesions is poorly known.
The typical appearances includes:
A multinational study of 2622 patients reported that these lesions are more common in women (1:4 ratio), avg age 58 yrs. In this cohort the size increased in 37% (growth rate: 4 mm/year), was stable in 57% and decreased in 6%. Only 3 serous cystadenocarcinomas were recorded and therefore a conservative approach was advocated. Most operations were carried out because of uncertainty over the diagnosis. Some would also consider offering surgery for patient with symptoms. However, in the above series only 9% of patients presented pancreaticobiliary symptoms directly related to the lesion. Because 10 patients died following surgery every effort must be made to make the diagnosis with the aid of CT, MRI and EUS and FNA. Low CEA levels with have an excellent specificity for diagnosis of a 'SCN' but can also be found in IPMNs and in neuroendocrine tumours.
Prof Saftoiu and his team will be uploading further EUS cases in their new FB group 'Friends of Endoscopic Ultrasound' ! |
Categories
All
|