|
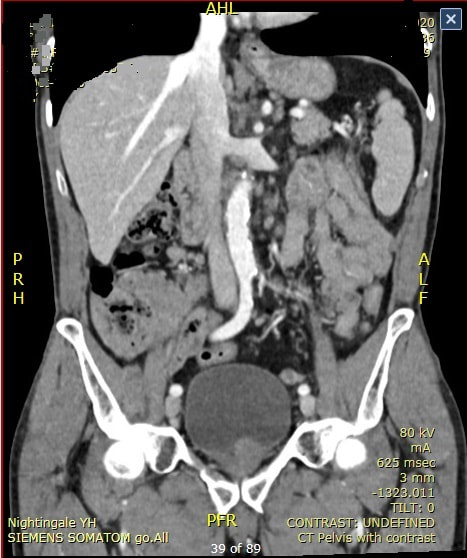
I'm carrying out a dilatation (20mm) of a distal gastric stricture. WHAT IS THE LIKELY AETIOLOGY OF THE STRICTURE?
■ Benign pyloric stricture
But the stricture is pre-pyloric!
■ Anastomotic stricture
Doesn't look like an anastomosis!
■ Radiotherapy stricture
But why giving radiotherapy to the stomach?
explanation
The mucosa in the 4 o'clock position looks pale and atrophic. This is a 'scar' left after treatment of a gastric lymphoma. Of course, the scar would look the same following Hp eradication of a MALT lymphoma. However, this was after following chemoradiotherapy (CRT) for a 'Diffuse large B-cell lymphoma. Which is a far more nasty lymphoma and patients present with more advanced stage at diagnosis, and have a worse prognosis (about 75% of patients are alive at 5 yrs) than with a MALT lymphoma. This patient was treated with 6 cycles of R-CHOP chemotherapy and radiotherapy 30 Gy in 15 fractions. The risk of stricturing after gastric CRT is around 5%. My dilatations to 20mm didn't do much and the patient had to come back for a dilatation to 25mm before symptoms improved.
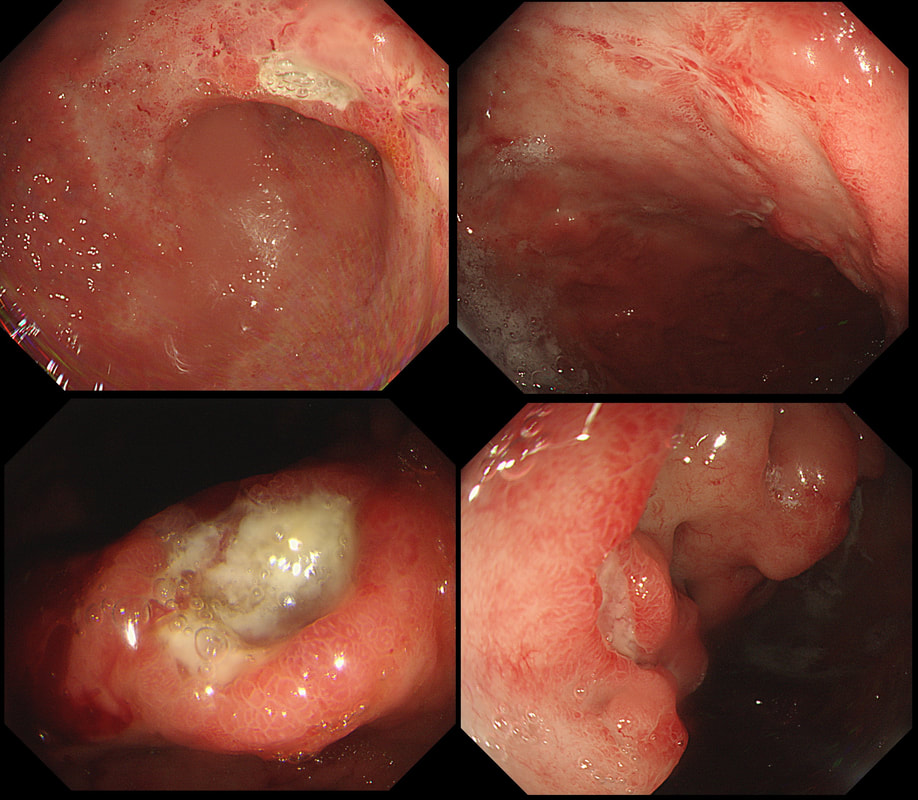
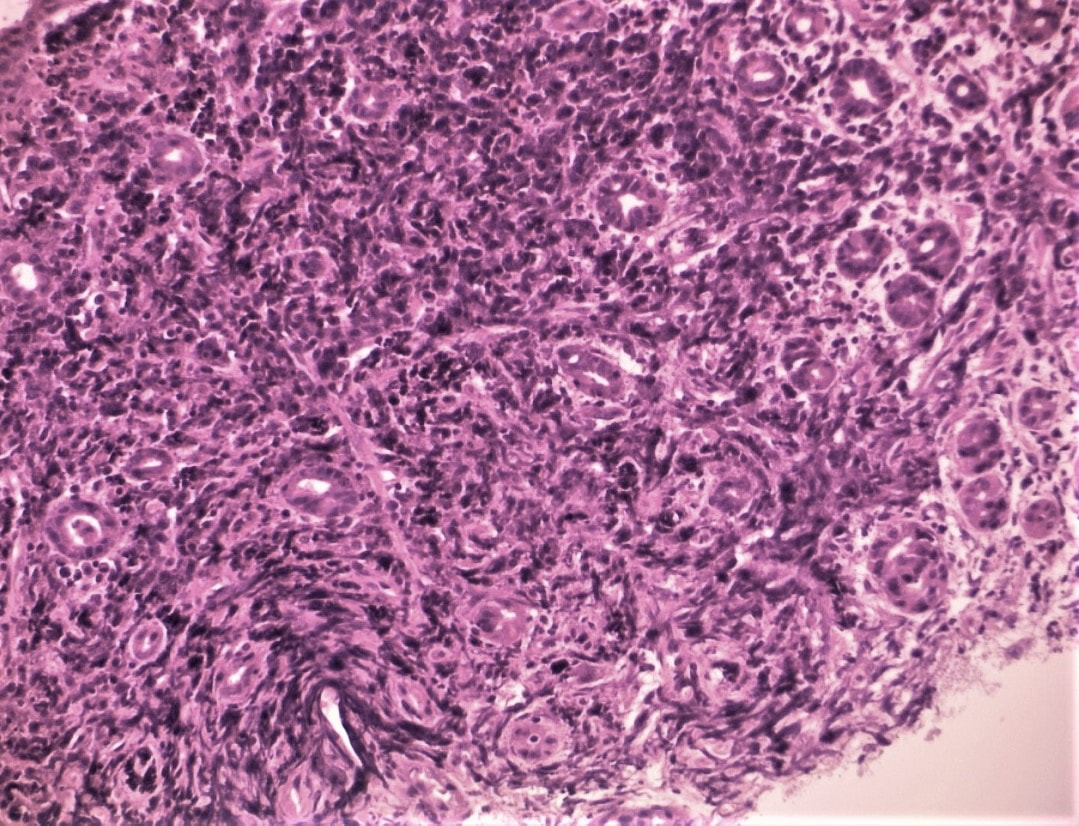
This ulcer was found on the lesser curve of a middle aged man with dyspepsia. Biopsies are taken and stained with H&E (below)
WHAT IS THE AETIOLOGY OF THAT GU?
■ Benign GU
Don't you think that the mucosa look odd near to the ulcer?
■ Lymphoma
Yes! That odd atrophic mucosa next to the ulcer look weird but not "carcinoma weird" !
■ Adenocarcinoma - intestinal type
With a 'standard cancer', the surrounding mucosa should be thickened and red not atrophic looking
■ Adenocarcinoma - intestinal type
This was actually my own diagnosis but histology shows lots of small round lymphocytes not ballooned up signet ring cells.
EXPLANATION
There are only two possibilities here. Of course the ulcer itself doesn't tell you much. The mucosa surrounding the ulcer tells you more! With a benign ulcer, you would expect a thin rim of 'reactive' mucosa (looks red and a little villous). In the case of an intestinal type of adenocarcinoma a broad band of surrounding mucosa is red, indurated and thickened. In gastric lymphomas, the surface area of abnormal mucosa is usually far greater than the surface area of the ulceration. There are usually areas of atrophic and inflamed mucosa. Mucosa infiltrated by a diffuse type adenocarcinoma could look like this BUT it's unusual for it to ulcerate!
This patient has a MALT lymphoma ! Of course, I took samples for Helicobacters. Of course not every MALT lymphoma is linked with HP infection (about 2/3 cases are though). In this case our haematologists were optimistic of a good response to Hp eradication because all the 3 good prognostic criteria were met:
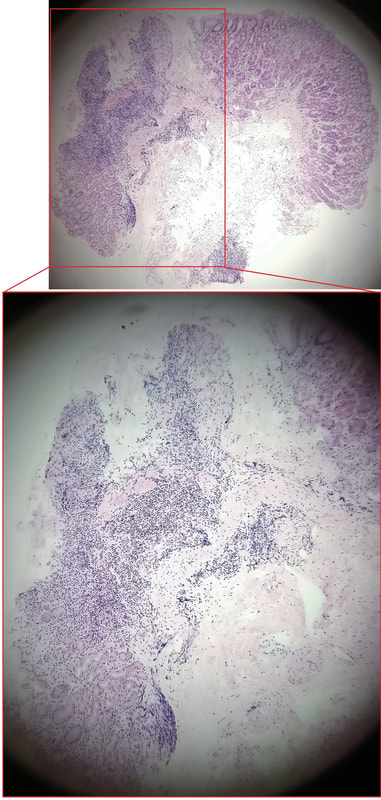
This polyp was found at the apex of the caecum. With some trepidation, a sample was obtained following which I requested the above CT
WHAT IS THE FINAL DIAGNOSIS ?
■ Hyperplastic polyp
Seems unlikely?
■ Inverted appendix
Was my very first thought too!
■ Adenoma
But I can't see a crypt pattern?!
■ Lymphoma
Why do you say that?
■ Mucocoele of the appendix
Was my diagnosis too and why I requested the CT!
explanation
I feel that I should apologise because it's almost impossible to make a diagnosis from the appearance of that appendix. The only abnormality, apart from it being there in the first place, is a subtle nodularity with a normal overlying mucosa. perhaps this rings a faint bell ???
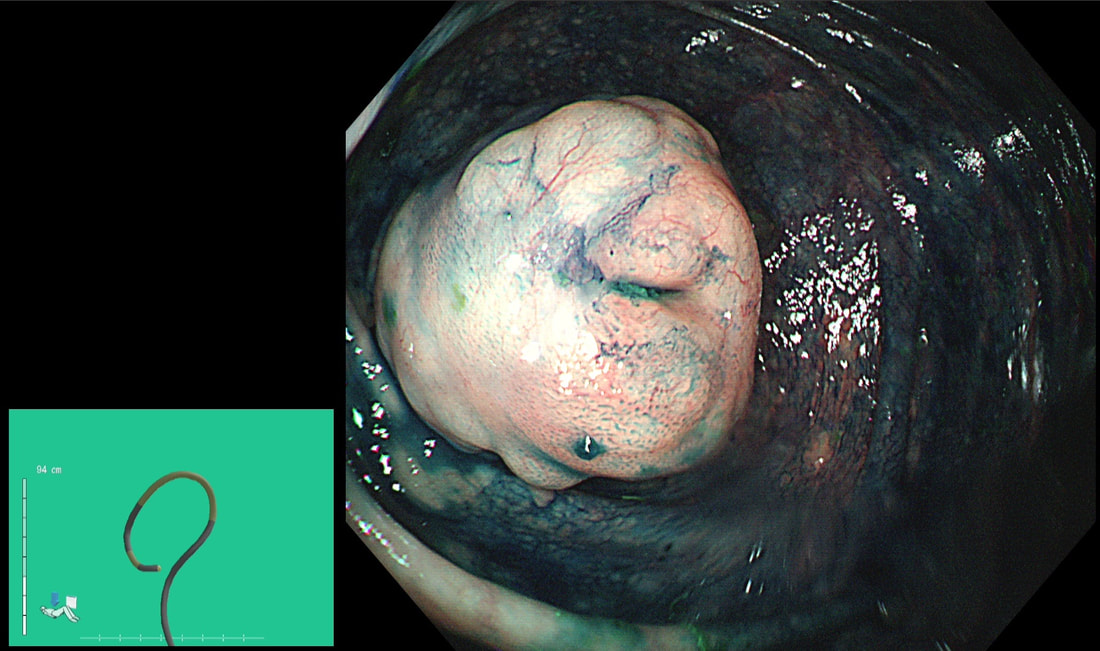
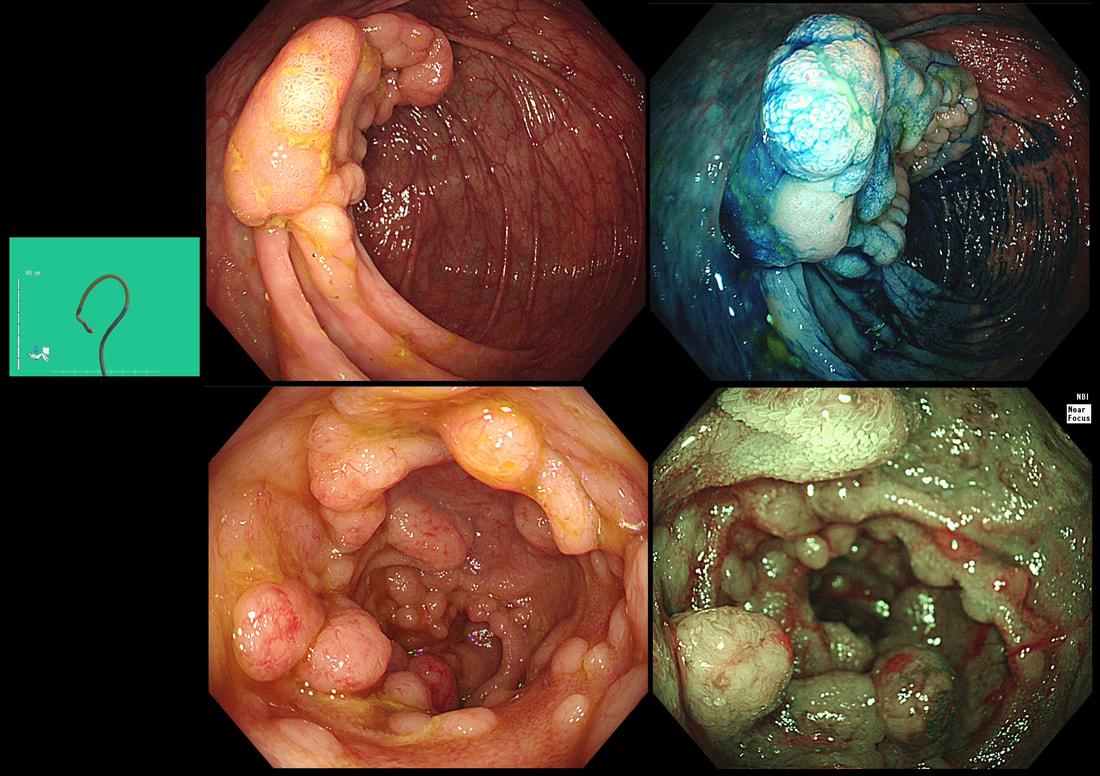
Actually, it turns out that the submucosa is full of small lymphoid cells clusters, forming balls. This is the classical histological appearance of a Mantle Cell Lymphoma? Mantle cell lymphoma has a predilection for the GI tract as the most common extra-nodal site. Indeed, one study found lymphoma in mucosal biopsies in 56/60 patients (both in UGI and Lower GI tract). This has given rise to a theory that mantle cell lymphoma actually originate from gut B-lymphocytes within the mantle zones of mucosal lymphoid follicles [Cancer 2003;97(3):586–91]. Endoscopic findings includes nodules, polyps, ulcers, and masses. I try to remember Mantle Cell Lymphoma if the mucosa appears markedly bumpy - as if the lymphoid follicles have gone crazy! In this case, the CT shows lots of enlarged lymphnodes, both above and below the diaphragm and the patient was started on 'Ibrutinib'. It's not a 'good lymphoma' as median life expectancy is only 6-7 yrs. This patient was undergoing colonoscopy because of abdominal pain, weight loss and suspected thickening of the terminal ileum seen on CT WHAT IS YOU ENDOSCOPIC DIAGNOSIS? a) Crohn's disease b) Adenocarcinoma c) Lymphoma d) Neuroendocrine tumour e) Tuberculosis explanation
Endoscopically, there appear to be 'nodules' arising from below the overlying mucosa. When I first showed this case, almost everyone correctly identified this as a case of lymphoma. Of course, MALT lymphoma in the stomach looks completely different with thickening and reddening of the gastric mucosa, usually with ulceration of the surface. The reason why this looks entirely different to a gastric MALT lymphoma is because it is a completely different type of lymphoma! Histologically, the submucosal nodules were made up of small to intermediate sized lymphoid cells clusters, forming solid sheets and balls. This is the classical endoscopic appearance of a Mantle Cell Lymphoma (MCL). MCL is a type of non-Hodgkin's lymphoma which arise within the 'mantle zone' that surrounds normal lymphoid follicles. It's presumably for this reason that endoscopically it looks like gross case of nodular lymphoid hyperplasia. It's not a 'good lymphoma' as median life expectancy is only 6-7 yrs. In this patient, a CT confirmed that there were large nodes both above and below the diaphragm. Although he had no symptoms our haematologists have started treatment with 'Ibrutinib' to reduce the risk of small bowel obstruction. From today, you will all recognise the typical endoscopic appearances of a MCL ! |
Categories
All
|