|
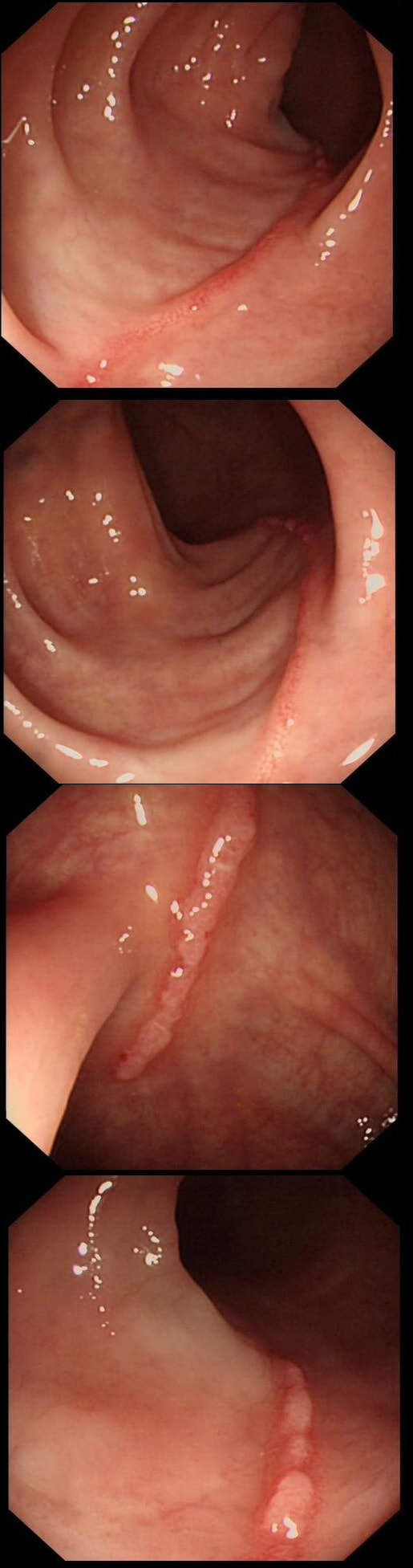
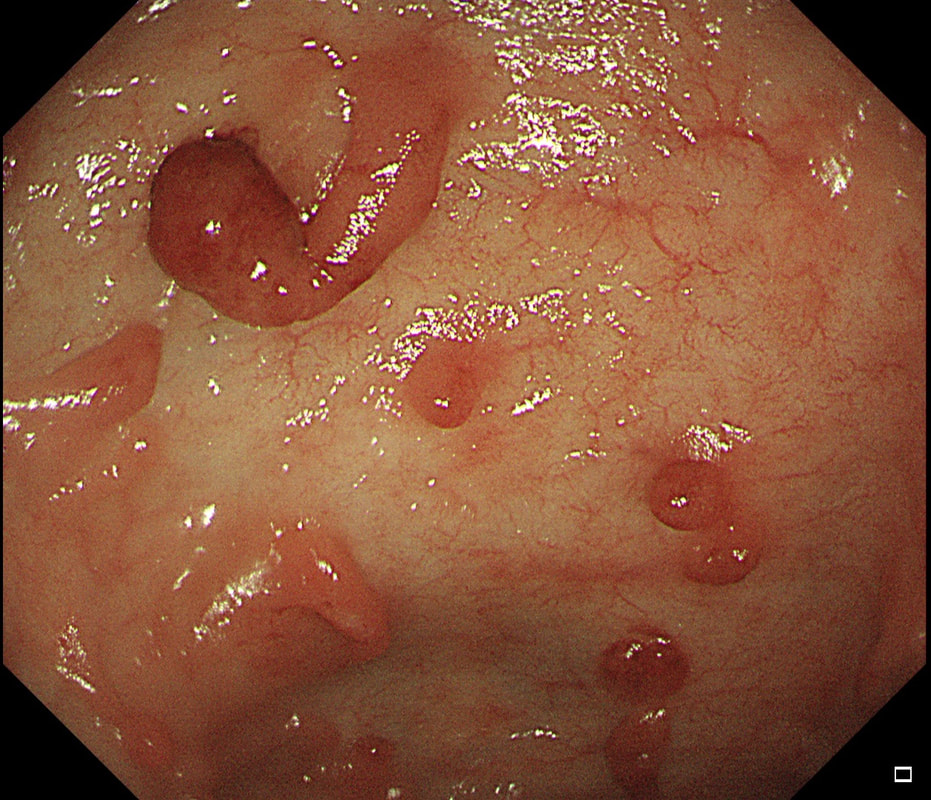
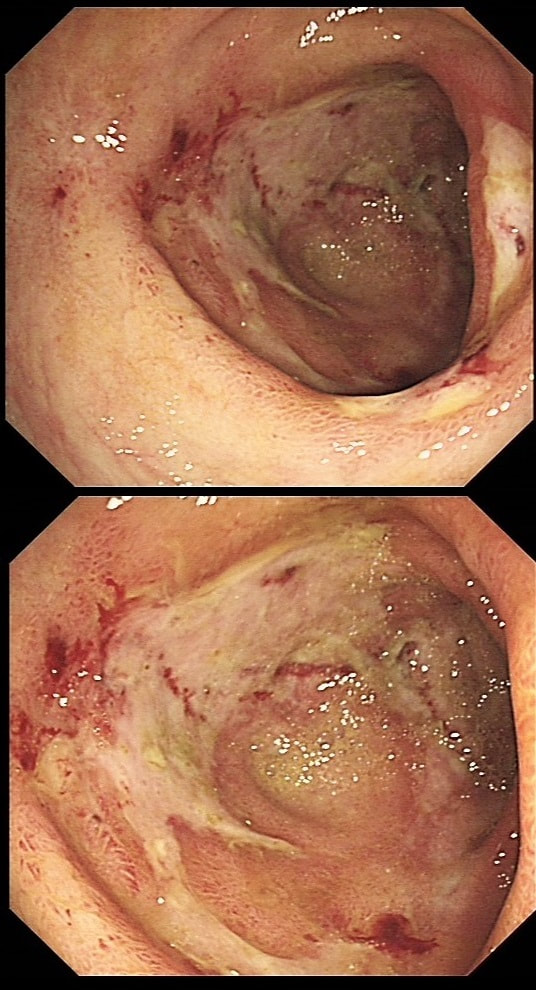
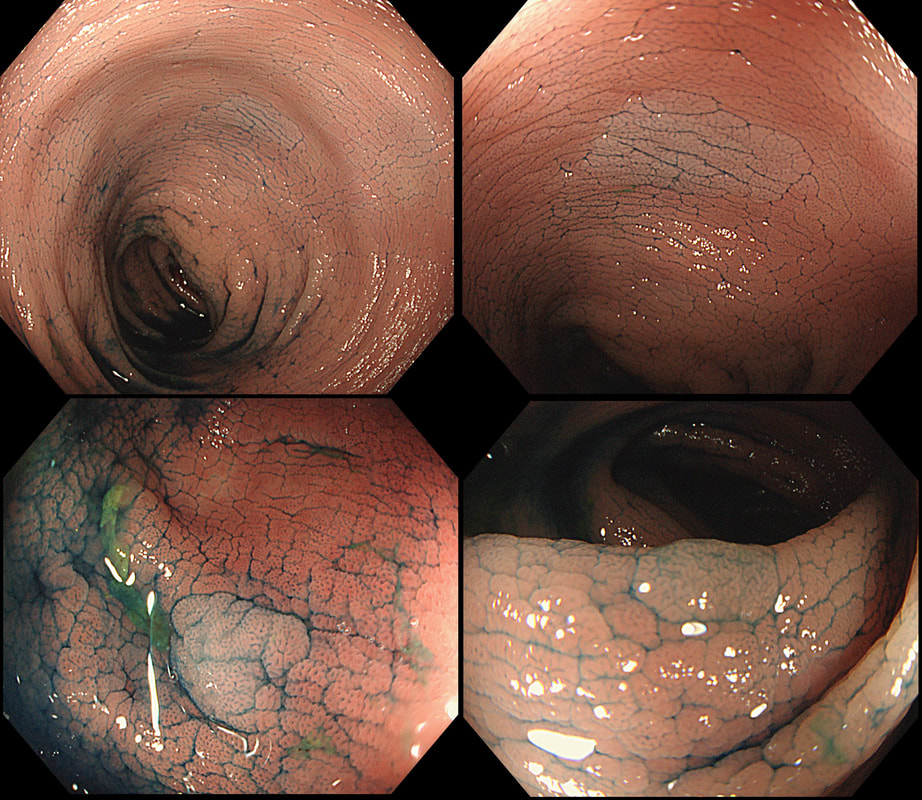
These linear lesions were found in a 50 yr old patient undergoing colonoscopy to investigate her loose stool.
WHAT IS THE LIKELY DIAGNOSIS?
a) Crohn's disease
Does give linear ulcers but should be larger and deeper!
b) Ischaemic colitis
Also gives linear ulceration, often on the ante-mesenteric border.
c) Collagenous colitis
Absolutely!
d) Ulcerative colitis
Doesn't give linear ulceration and surrounding mucosa wouldn't be normal
e) Lymphocytic colitis
Perhaps one could develop into the other?
explanation
Actually, this patient had collagenous colitis! I suspect that the acute injury are linear tears in the mucosa which then granulate as in the images above. Finally, you are left with linear scars as in the image below. Pure speculation but seems logical ! At colonoscopy, the mucosa is often unremarkable but there may also be mild, patchy erythema or linear cracks. Histology reveals the typical thickening of the subepithelial collagen layer from the normal 3-6 μm to more than 10 μm as well as lymphocytic infiltration of the epithelium and the lamina propria. Rectal biopsies are not sufficient to make the diagnosis as normally the collagen layer is particularly thin here. Samples from the rectum and sigmoid confirms the diagnosis is more than 90% of cases. Interestingly, patients with eosinophilic oesophagitis may also develop some fibrosis in the lamina propria which also 'cracks' in a spectacular way when a dilatation is carried out.
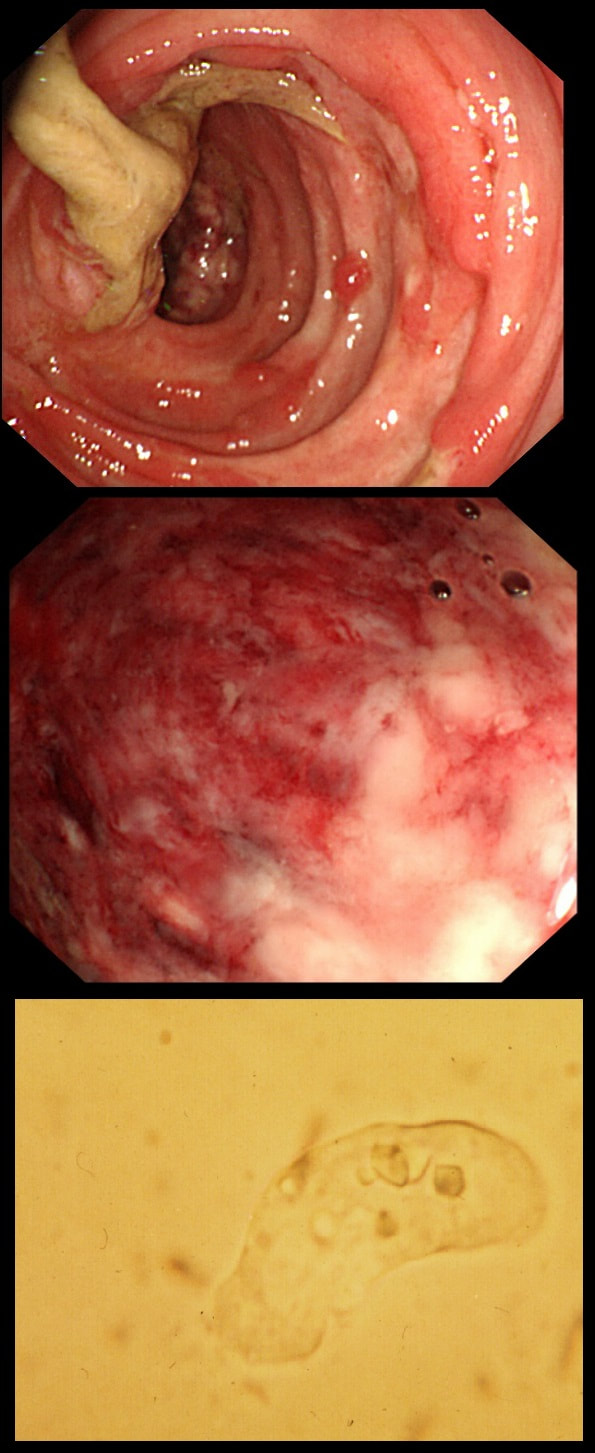
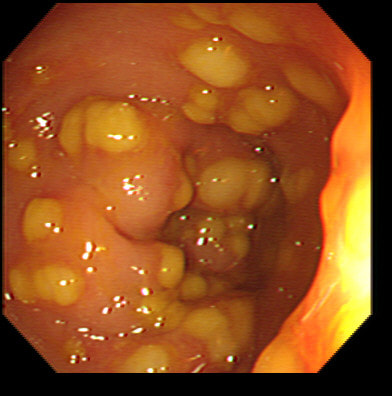
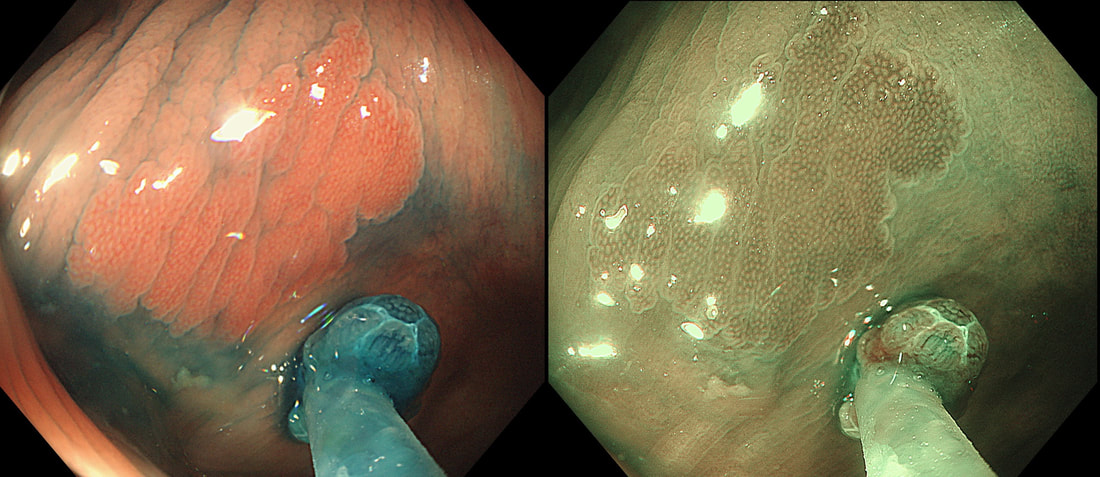
This patient developed bloody stool whilst on holiday in Africa. They continue on return home and he undergo a flexible sigmoidoscopy. Of course, stool samples are obtained (last image).
WHAT IS THE PATHOGEN?
a) Clostridium difficile
Can be seen moving down a microscope
b) Salmonella enterica
Can give bloody diarrhoea but its not it!
c) Entamoeba histiolytica
Rasberry stool, to be examined warm
d) Campylobacter jejuni
May also give bloody stool but that's not it
e) Vibrio cholerae
Hmm, rice-water stool...
explanation
Let me give you some more clues! Classically, there are 'flask-shaped' ulcers found on resectional histology in which the mucosal surface ulcer is rather narrow with a wider, necrotic submucosal component in which the amoeba multiply. Stools have been described as like "Raspberry jam" and when examined whilst still warm, something can be seen moving. Of course PCR is the best way of confirming the diagnosis.
This patient had amoebic dysentery! Mild cases can resolve without metronidazole.
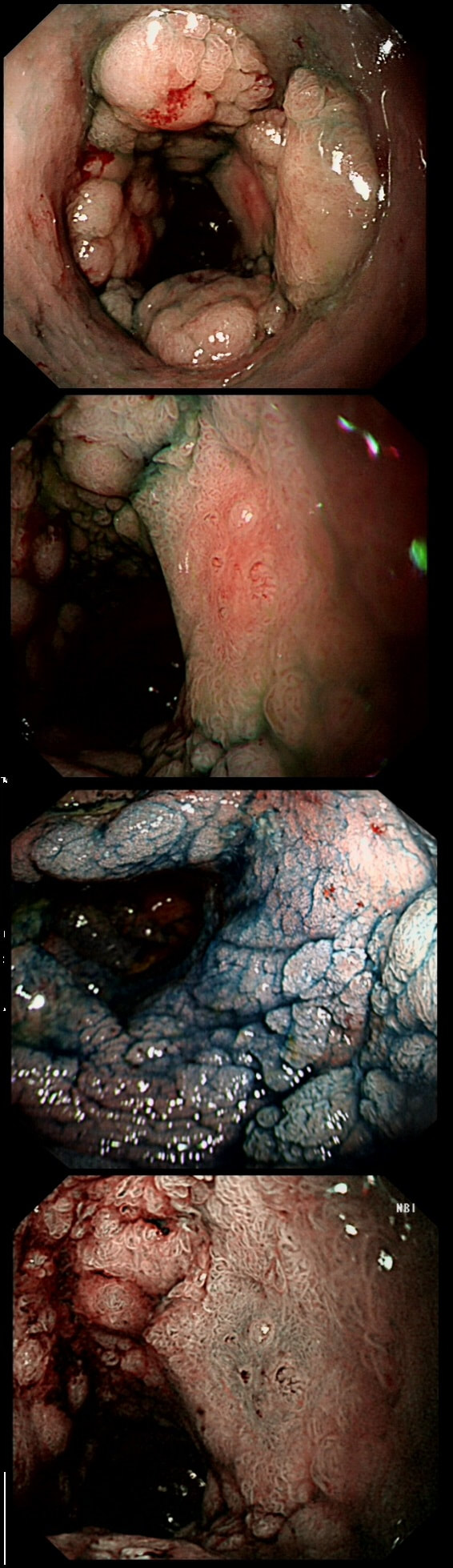
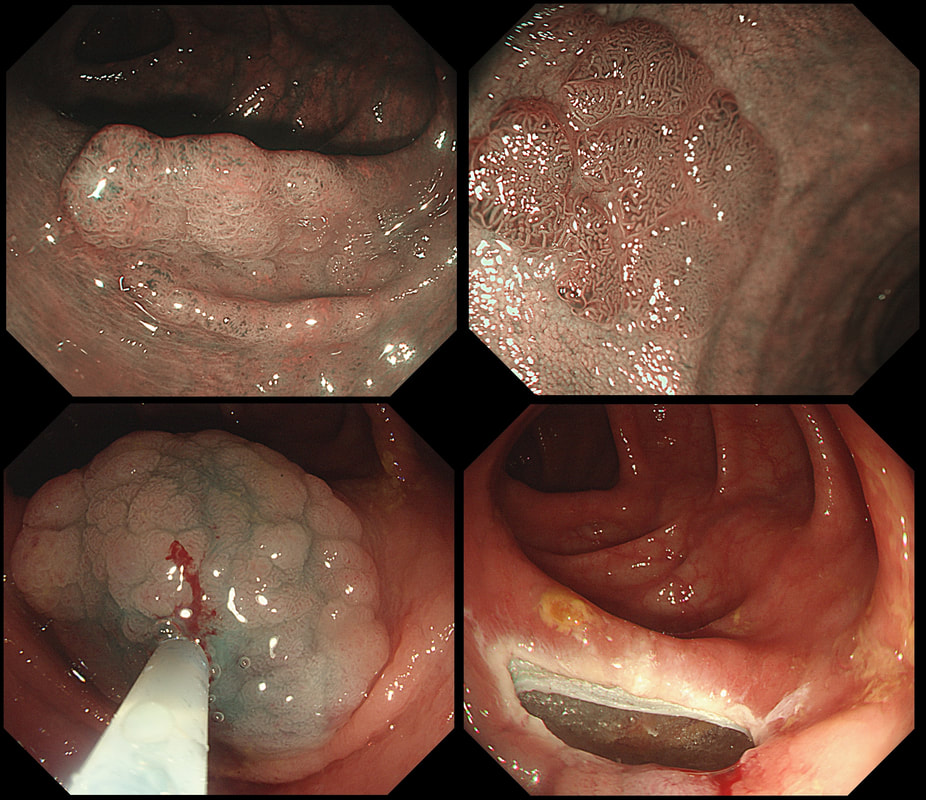
This patient with ulcerative colitis has developed a polyp in the transverse colon. The lesion has now been sent for an endoscopic resection.
WHAT WOULD YOU DO?
a) Abort!
Smart!
b) Attack!
You are creating a problem of your own making!
explanation
Some would say; "if you can remove the lesion in that colitic colon, then 'do it'! The problem is that nothing may appear "irresectable" giving plenty of time, determination and poor judgement.
Many studies looking at outcomes of polypectomy in UC, excluded polyps >1-2cm or flat polyps. Other studies have included polyps arising outside of the colitic field or only have a short follow up period of a few years. Actually, most are coming to believe that when dysplasia develops in the colitic colon, it's not a 'random' case of bad luck. It can be the result of a long process of progressive DNA damage! At some stage we will be able to have a look at the state of the stem cell DNA in patients with conditions such as Barrett's, Colitis and atrophic gastritis. I think that we are in for a surprise ! In addition, did you spot the small focus of invasive cancer in the 2-3 O'clock position? Surprisingly, this was only T1 disease!
These peculiar colonic lesions were found in the colon of an asymptomatic patient.
WHAT ARE THEY?
■ Inflammatory polyps
Absolutely!
■ Adenomatous polyps
These are too long and peculiar looking to be adenomatous!
■ Hamartomatous polyps
No way!
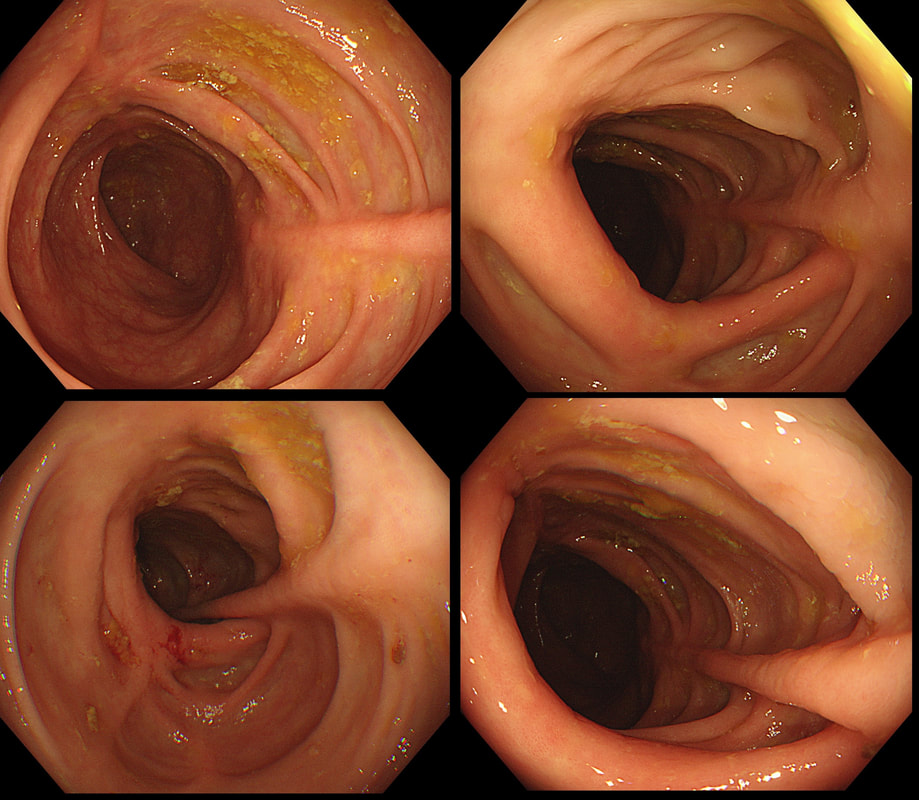
This 80 yr old man was first referred for a CT to investigate his PR bleeding and mucus. The CT reported that the rectum appeared thickened and a Flex Sig is organised WHAT IS YOUR DIAGNOSIS?
■ Active proctitis with inflammatory polyp
That was my diagnosis and I was half correct!
■ Active proctitis with adenomatous polyp
Very good call!!! Better than mine if fact!
■ Circumferential polyp with dominant nodule
Apologies for the indigo carmine dye which has confused you!
■ Circumferential polyp with malignant change
The blue dye is confusing and the proctitis does look weird in places
explanation
Yes, it does seem odd to refer for a CT rather than a Flex Sig? Perhaps this was because the patient was 80 yrs old or because of our endoscopy waiting list. Anyway, I was half correct. I diagnosed an active colitis and histology confirmed a: transmucosal inflammation with crypt abscess and focal epithelial loss (tiny, tiny ulcers). We all know that active colitis is characterised by an dull erythema, bleeding and erosions/ulcers. The best endoscopic scoring system is currently the Ulcerative Colitis Endoscopic Index of Severity (UCEIS) which scores these three parameters on a scale of 0 to 3. There are other scoring systems of course such as the Mayo score, the Baron score, The Rachmilewitz Endoscopic Index, The Sutherland Index, The Matts Score, The Blackstone Index and the most recent addission, The Ulcerative Colitis Colonoscopic Index of Severity! Of course this tells you than none of them is the last word on the topic. For a good review of all endoscopic issues relating to colitis, please check this article out; Annese V. European evidence based consensus for endoscopy in inflammatory bowel disease, J Crohn's Colitis 2013;7(12);982-1018 Anyway, I find it odd that other common features of an active colitis are not included in any of these scoring systems. This includes mucosal oedema, a villous epithelial surface (as seen in this video) and a mucopurulent discharge (which I regard as feature of a severe attack of colitis). These three features are prominent in this video and if not recognised as features of an active colitis, can be mistaken for a neoplastic process. I thought that the nodule would be inflammatory but it turned out to be a 'TSA' (traditional serrated adenoma), the most rare and elusive of all colorectal polyps. Well I blame the inflammation and that thin mucopurulent layer obscuring the crypt pattern. This is the sigmoid colon and rectum of a young patient who have just undergone bone marrow transplantation. WHAT IS THE LIKELY DIAGNOSIS?
■ Graft versus host disease
You don't get ulcers in GVHD!
■ Checkpoint inhibitor colitis
You DO get ulcers with these but they wouldn't be used!
■ Pseudomembranous colitis
Doesn't cause ulceration
■ CMV colitis
Absolutely !
■ Herpetic colitis
Hmm, does this actually happen?!
explanation
In GVHD there are minimal mucosal changes whilst there is extensive ulceration in this case. You do get nasty mucosal ulceration with checkpoint inhibitors but these drugs would not be used in transplantation. C.diff doesnt' cause mucosal ulceration and the herpes virus does not infect columnar mucosa. This leaves CMV ! Cytomegalovirus is a herpes virus that infects the majority of humans. Primary infection in individuals with normal immune function is usually asymptomatic or result in mononucleosis-like syndrome (fever, lymphadenopathy, and atypical lymphocytosis on a blood film). After primary infection, CMV becomes latent in various host cells but are controlled by a functioning immune system. When re-activation occurs in patients with severely compromised immune function (transplant patients or patients with AIDS and CD4 count <50 cells/microlitre), uncontrolled CMV replication can ensue leading to fever, bone marrow suppression, and tissue-invasive disease, depending on where the reactivated cells are residing. Investigations includes serology, pp65 antigenaemia test, histopatholical analysis of any tissue obtained, and PCR based detection. Treatment of choice is oral valganciclovir or intravenous ganciclovir whilst IV foscarnet and cidofovir are second line agents.
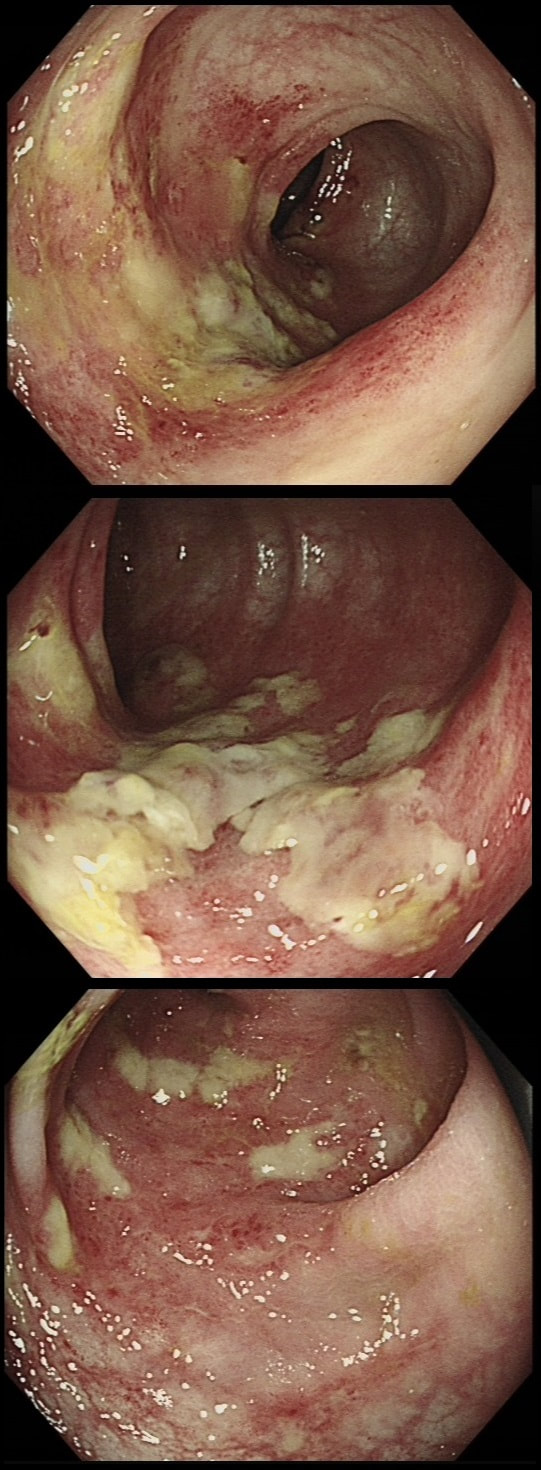
This is the sigmoid mucosa of an elderly inpatient who has developed diarrhoea.
WHAT SINGLE TEST WOULD YOU RECOMMEND NEXT?
■ FBC
Of course it's not sensitive nor specific and does not exclude diagnosis if normal. Nevertheless, a very high WBC level is often found in fulminant pseudomembranous colitis.
■ Obtain a set of stool cultures
Probably not a priority and they should have done it already!
■ ELISA for C.diff toxin in the stool
Yes! Results available within a few hours with sensitivity of 65%-85% and specificity 95%-100%
■ Stool PCR for C.diff
Seems like a sensible investigation in patients with unexplained, new-onset diarrhoea but perhaps not the single most important test...
■ Abdominal X-ray
Important IF there is significant abdominal distension
explanation
Of course this is a case of Clostridium difficule associated colitis (pseudomembranous colitis). Patients usually present with diarrhoea, abdominal pain, and leukocytosis, and a history of recent antibiotic use. Other common symptoms include fever, abdominal tenderness, and distension.
In a symptomatic patient with typical colonic pseudomembranes such as in this case, arguably it would be sensible to recommend that treatment is immediately started. Stool testing should be considered in any patient with unexplained, new-onset diarrhoea (defined as 3 or more unformed stools in 24 hours in a patient not taking laxatives). Your local institution will probably have protocols for how patients should be investigated and all of the above test may well be part of the algorithm. When I was on the wards, toxin tests were favored over culture for diagnosis of C.diff because it was the toxins which mediate disease. detection of toxins was faster and correlated better with symptoms. However, there was a move towards 'molecular tests' (PCR for the bacterium) from 2009 because of concern that patients with C.diff could be missed by toxin tests. Of course, this raised the question; do toxin-negative patients with a positive C difficile PCR test result require treatment? Several studies have now indicated that about half of the patients with positive PCR test for C. diff do not experience adverse events without treatment and do not need treatment. For this reason, PCR testing for C.diff should not be used as the stand-alone diagnostic test. Instead it's patients with clinical disease (diarrhoea) AND a positive toxin assay who should be treated! There are lots of references for this statement and here is an open access article in JAMA: Treatment is to discontinue the responsible antibiotic and start therapy with oral vancomycin or fidaxomicin. Up to 50% of patients have a relapse after discontinuation of antibiotics, but most respond to a second course of therapy. In those who relapse again, faecal microbiota transplantation is very effective.
This is the colon of a 55 year old woman who has been treated for diarrhoea.
WHAT IS THE DIAGNOSIS?
■ Crohn's disease
Possible of course but why a 'middle aged lady'?
■ Ulcerative colitis
Zero points!
■ Microscopic colitis
Of course!
explanation
Actually, this patient had collagenous colitis and after treated with budesonide, symptoms settled. A colonoscopy 3 months later showed these linear scars throughout the colon.
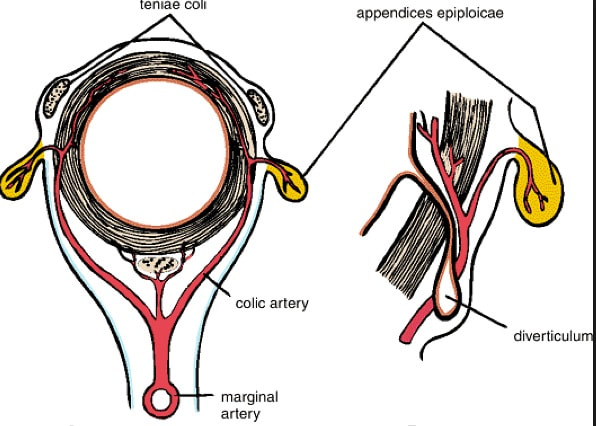
The first case of collagenous colitis was described in 1976 by Lindström and is characterised by chronic watery diarrhoea. Underlying hyperthyroidism, coeliac disease, bile salt diarrhoea and inflammatory bowel disease should be excluded. At colonoscopy, the mucosa is often unremarkable but there may also be mild, patchy erythema or linear cracks. Histology reveals thickening of the subepithelial collagen layer from the normal 3-6 μm to more than 10 μm as well as lymphocytic infiltration of the epithelium and the lamina propria (see image below). Rectal biopsies are not sufficient to make the diagnosis as normally the collagen layer is particularly thin here. Samples from the rectum and sigmoid confirms the diagnosis is more than 90% of cases. 9mg of Budesonide is effective but there is a high risk of relapse on stopping the drug [Bonderup OK. Gut 2003;52:248-51] and azathioprine is usually the second line agent. This was found in the sigmoid of a 35 year old lady presenting with abdominal pain and bleeding. She has been taking ibuprofen for her pain. WHAT IS THE MOST LIKELY DIAGNOSIS?
■ NSAID induced colitis
Possible but the pain came before starting the ibuprofen
■ Ulcerative colitis
Stricturing and linerar ulcers are not typical for UC
■ Crohn's disease
Most likely and don't forget to add your endoscopic diagnosis to the histology request form!
■ Diverticular stricture
Those rarely ulcerate and are usually MUCH tighter
■ Malignant stricture
Those post-inflammatory polyps are innocent!
explanation
The superficial, linear ulcers are typical of inflammatory bowel disease. Both ulcerative colitis and Crohn's disease can cause stricturing but of course Crohn's is more likely to. Those little nodules are post-inflammatory polyps, covered in normal crypts. In any case of colitis it's important to take a full set of samples, targeting not only areas which are visibly inflamed but also non-inflamed areas. Patchy inflammation is very suggestive of Crohn's disease but if you neglect to sample the non-inflamed areas, you will find that your pathologists will report a continuous colitis which would be more suggestive of ulcerative colitis. After all, they can only report on the samples given to them and may well not read your endoscopy report.
This 70 year old patient with known ischaemic heart disease presents with sudden onset bloody diarrhoea. He undergoes a flexible sigmoidoscopy the following morning and this is what the sigmoid colon looks like. With support and conservative measures symptoms subside and the patient is discharged a week later. However, a week later the patient presents again. Now with hypotension, abdominal distention, fever and a raised white count. An abdominal X-ray is done on admission (below).
WHAT IS THE LIKELY DIAGNOSIS?
■ Colonic stricture
Too soon for this!
■ Another attack of ischaemic colitis
Unfortunately, yes!
■ Pseudomembranous colitis
He didn't actually receive any antibiotics last admission
■ Crohn's disease
Unlikely !
explanation
There is little mystery that the first presentation was due to ischaemic colitis. The second presentation is more tricky. He actually presented with an ileus and pain this time. Actually, the patient had been on aspirin but this had been stopped at the previous admission. This was clearly a mistake as the second presentation turned out also to be due to ischaemic colitis. This time the ischaemic colitis was more severe but he did recover in the end.
After ischaemic colitis about 10% of patients develop and ischaemic stricture but it takes longer than a single week to develop. The hallmark of an ischaemic colitis are areas of longitudinal ulceration, on the anti-mesenteric border (90° to any diverticulum) where the blood flow is the slowest. Of course, endoscopically its difficult to tell where the omental reflection is situated. However, the ulceration will run along one aspect of the colonic circumference. Of course in the epicentre of the ischaemic (typically around the splenic flexure), the ulceration may well be circumferential. Ischaemic colitis is surprisingly easy to confirm histologically as the pathologists look for crypt withering and fibrosis. By the way, if the mucosa looks dusky and there is no bleeding on taking samples, the likelihood is that the colon is turning gangrenous, associated with a >50% mortality rate.
A 65-year-old man presents with a 1-week history of a worsening low abdominal pain. The abdominal pain was preceded by exertional chest pain that settled with anti-anginal therapy prescribed by the patient’s GP.
Apart from hypertension that is managed with ramipril, the recently started anti-anginal drug nicorandil and low-dose aspirin, the patient is well and able walk several miles without shortness of breath. Routine blood tests are normal on admission and the patient denies taking an NSAID or paracetamol. After the CT above and colonoscopy is carried out showing the above caecal inflammation. Unfortunately, the patient soon deteriorates requires an emergency right hemi-colectomy before histology is to hand. WHAT IS THE MOST LIKELY DIAGNOSIS?
■ Aspirin induced colitis
With 75mg of aspirin ?
■ ramipril induced colitis
Never heard of it!
■ Ischaemic colitis
An unusual but well recognised location but wrong ☺
■ Nicorandil induced colitis
Up to 5% get colitis on this drug
■ Crohn's disease
Nope, that's not it!
explanation
Getting this diagnosis wrong would have profound implications for the patient ! The ulceration would be likely to recur and the patient may even present with further ulceration unless it is recognised that the cause is his nicorandil tablets !
Nicorandil, a combined venous and arterial vasodilator is effectively the drug of last resort for angina. The reason is that there have been numerous reports of ulceration affecting skin, eyes or mucous membranes which have accumulated since the drug was launched in 1994. Small aphthous ulcers are said to occur in up to 5% of patients but more severe, painful and deep ulceration may ensue. In the gastrointestinal tract, perforations, fistula formation and abscesses are recognised complications. Patients taking NSAID’s, steroids or have diverticular disease are at particular risk. There is also some evidence that the risk of ulceration increases with dose and ulceration may be precipitated by an increase in dose. The underlying mechanism by which the drug causes ulceration is unknown. However, nicorandil-induced ulcers persist until the drug is withdrawn although healing may take up to 6 months. In addition to patients with a history of ulceration of mucosal membranes, nicorandil is contraindicated in patients with hypokalaemia, heart failure and renal impairment.
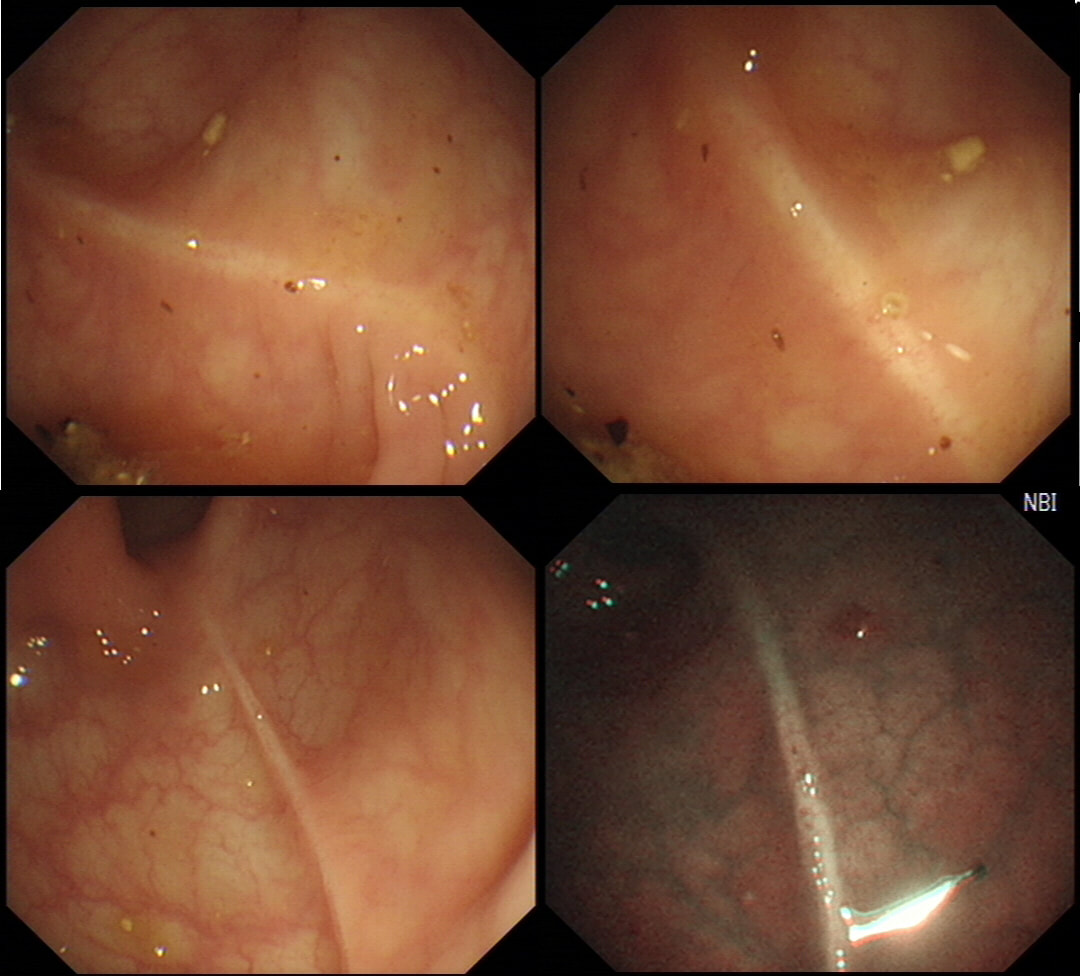
These linear lesions were seen within the left side colon of a lady undergoing colonoscopy because of loose stool. The patient denies taking any medication.
WHAT IS THE LIKELY DIAGNOSIS?
■ Post ischaemic colitis
Surprisingly (perhaps) not!
■ Post collagenous colitis
Well Done!
■ Post Crohn's colitis
Perhaps surprisingly, not!
explanation
These linear scars have been described (GIE 2010;71(1):221) in patients with both types of 'microscopic colitis' (collagenous colitis and lymphocytic colitis). Presumably it's because the lamina propria can be fibrotic, which makes the mucosa "brittle" and prone to superficial cracks. When I see these fresh cracks (example below, courtesy of Dr Gareth Davies), in the right hemi-colon of a patient with microscopic colitis, I always thought that I have insufflated too hard. However, they can evidently happen spontaneously and then heal as linear scars. In this case, the subsequent histology confirmed our endoscopic diagnosis of a microscopic colitis.
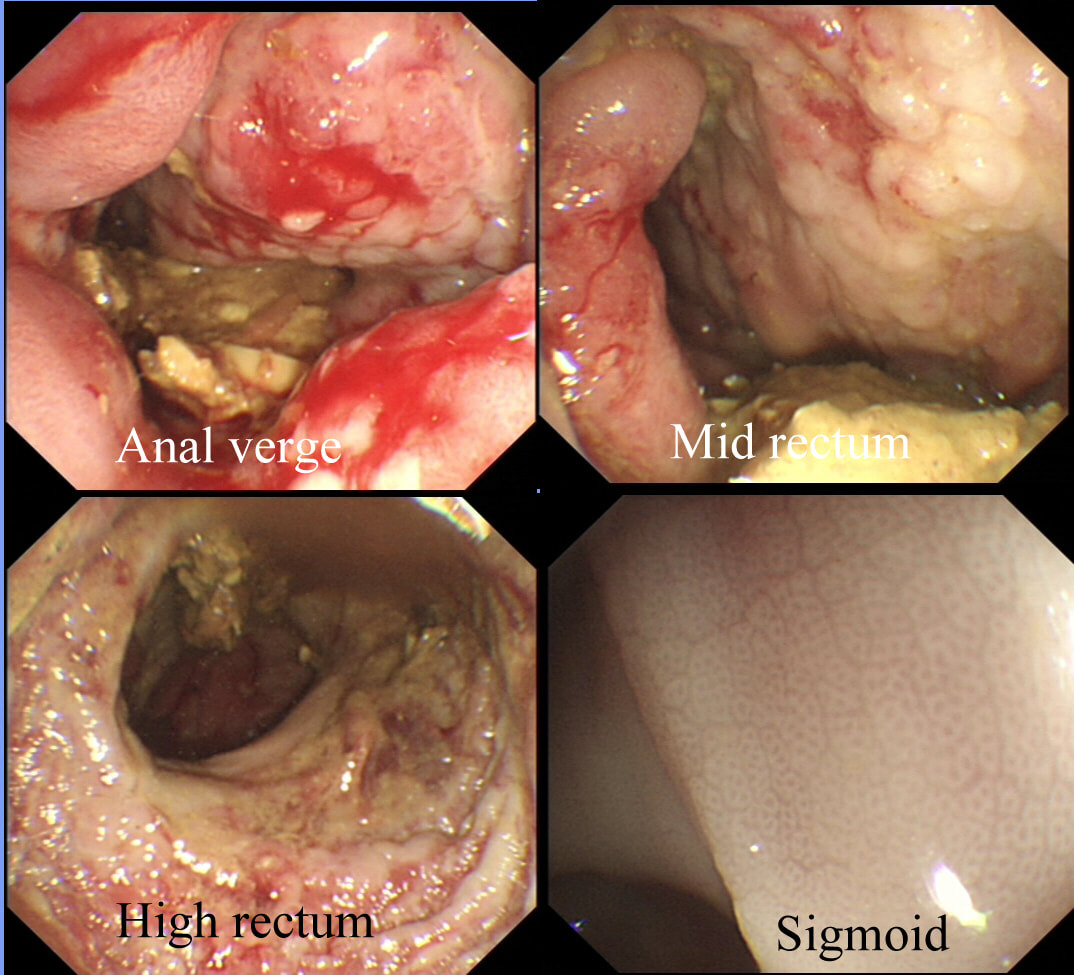
This is the rectum in an elderly patient admitted following a stroke a weeks ago. A week after admission she started to complain of pain around the tailbone. A CT reported that the rectum was "non-specifically inflamed". This turned out to be an understatement (!) as the rectal mucosa is actually almost completely ulcerated from the anal verge up to the sigmoid junction! The sigmoid mucosa looked a little pale and oedematous but the patients albumin was only 22 g/L. There is no history of NSAID use. There is no known vascular disease and no past history of radiotherapy to the prostate.
WHAT IS THE DIAGNOSIS?
■ SOLITARY RECTAL ULCER SYNDROME
INCORRECT!
■ CROHN'S COLITIS
Nope!
■ ULCERATIVE COLITIS
Unfortunately not!
■ STERCORAL COLITIS
YES, you are right !
■ ISCHAEMIC COLITIS
No, the rectum has a HUGE blood supply!
explanation
I had just scoped this patient and knew that I was missing something important. Why did his rectum look such a mess?!!
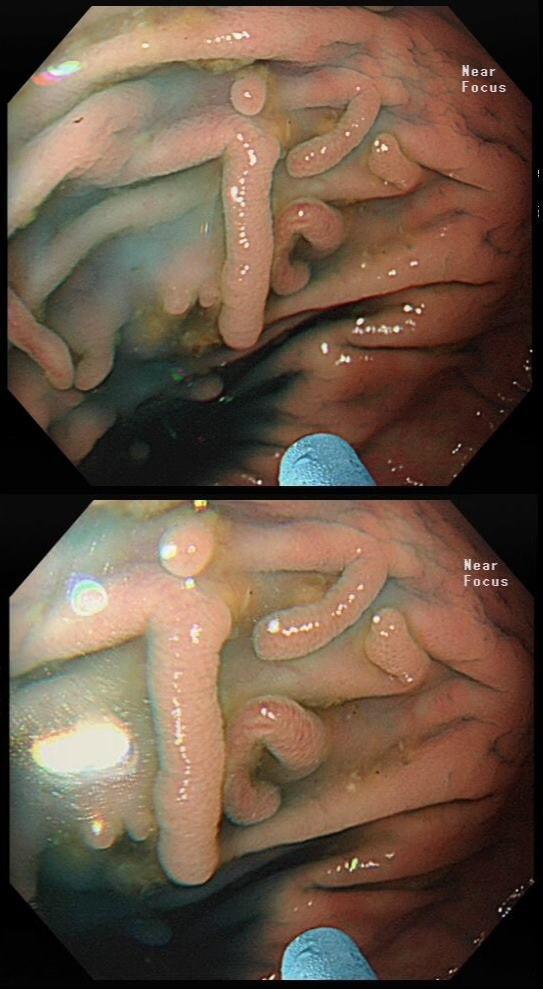
Uploading the history and images onto FoE, I didn't wait for more than 20 minutes when Pete Basford (Consultant at Southlands Hospital) suggested a 'stercoral colitis'! The Power of Friends of Endoscopy !!! The opinion of thousands of experienced doctors with a particular interest in Endoscopy available on your phone. Awesome ! Both CT and histology was of no use whatsoever just reporting 'severe rectal inflammation and ulceration'. Nobody had 'joined the dots'! Of course, the diagnosis is clinical, relying on recognising the pattern of a constipated, bedbound patient with severe rectal ulceration. Of course, when the patient turned up for a flexible sigmoidoscopy, the rectum was empty because of the enema! An under recognised diagnosis! Impacted faeces lead to local pressure necrosis and the increased rectal pressure gives rise to mucosal ischaemia. It's most common in the sigmoid and rectum because this is where the colonic pressure is the greatest. Remember that the ulceration can be patchy. Of course it most commonly seen in elderly immobile patients with a history of chronic constipation, dementia, or inpatients immobilised after a stroke or who has been rendered bedbound for other reasons. The feared complication is perforation which is usually fatal. This is the colon of a patient with long-standing colitis and PSC on annual surveillance. These were found after indigo carmine dye spray. WHAT IS YOUR ENDOSCOPIC DIAGNOSIS? a) patches of crypt distortion b) serrated lesions c) a flat adenomas Explanation
Actually, these are patches of 'crypt distortion'. Often seen after pan-colonic dye spray and VERY difficult to distinguish from serrated lesions. The crypt openings are a little larger than normal and strangely these seem to develop in patches which can be very large. In a case like this, I would take samples to reassure and alert subsequent surveillance colonoscopists to the presence of these odd lesions. In my experience they are usually seen in long standing colitis which has been troublesome in the past and I wouldn't be entirely surprised if future research find that these are more commonly found in patients who go on and develop flat dysplasia in the future. Below is a close-up of a lesion.
This polyp was found in the transverse colon in a patient with long-standing ulcerative colitis. WHAT WOULD YOU DO NEXT? a) retrieve the polyp and look for other polyps b) obtain 4 samples from the nearby mucosa c) apply APC to the EMR edges d) tidy the edges up with a cold snare e) apply clips Explanation
That hole isn't right! More often than not, this is how a perforation looks immediately after polypectomy. As a beginner you may think that you should be able to see the peritoneum but that would be the exception. Must admit that I was surprised to see this perforation. The lift seemed to be good and I didn't use a 'super-stiff' snare. Perhaps it had something to do with the fact that the patient had colitis? Because the 'cutting' should have taken 6-7 seconds but took about 12 seconds, I did expect 'trouble' and had started to suck air out of the colon before the snare cut through completely. Fortunately, the colonic lumen is not deflating as the perforation is close to the omental reflection. We will have a few minutes before the patient starts to become uncomfortable. Spend those minutes well !!! I applied 10 clips. The colon was clean and I was confident that there was no peritoneal contamination. Of course, this is one of the reasons why your polypectomy site should be as dry and clean as possible before you step on that yellow pedal! There was no pain and after a couple of hours in recovery and I discharged the patient with verbal and written instructions to return to A&E if pain developed later. The patient was fine. Can I reassure you that every patient will be fine after closing a perforation by clips? Of course not! You need to follow your instincts and your local protocols and of course be able to defend your decisions. Naturally, the particulars of the actual patient is very important. For example, an elderly patient or someone living alone should probably not be discharged. After all, sepsis can develop quickly and the patient may soon be in no fit shape to call for help. This patient was brought down from the haematology ward with diarrhoea. The patient was immunosuppressed following a donor bone marrow transplant for myeloma. WHAT IS THE LIKELY DIAGNOSIS? a) Graft versus host disease b) An opportunistic infective colitis c) Checkpoint inhibitor colitis explanation
This is a case of acute Graft-versus-host disease (GVHD). Checkpoint inhibitor colitis gives a severe looking colitis whilst superficial ulceration is what should make you consider an opportunistic infective colitis. In the case of GVHD, there is usually very little to see. I knew that GVHD was due to T cells from the stem-cell donor which attack tissues in the recipient. However, I hadn't realised that it's the main cause of death after a stem cell transplant! This is bad news! The most common tissues affected by acute GVHD are the skin (widespread rash even appearing on the palms of the hands), liver (transaminitis) and the gastrointestinal tract. The horrendous secretory diarrhoea, classically developing in the weeks following a stem cell transplantation, is the most severe complication and linked with the 40% mortality rate of acute GVHD. There are a few take-home messages for endoscopists. ■ First, is that the mucosa may appear entirely normal but that samples nevertheless have to be taken as the diagnosis is clinical (of course) and histological (apoptosis of epithelial cells with loss of crypts). ■Secondly, endoscopic appearances are variable ranging from oedema (as in my video) to small intramucosal haemorrhages to erosions and ulceration. There is something called the 'Freiburg Classification' which basically orders this into a 4-level scale: 1 Normal mucosa 2 Patchy erythema 3 Aphthous ulcers and/or focal erosions 4 Confluent ulceration ■ Thirdly, 10 biopsies from the distal colon have the greatest chance of yielding the diagnosis. I take 3-4 biopsies from the rectum and sigmoid and if possible also the descending colon. ■ Fourth, because of the horrendous diarrhoea, there is no need to subject the poor patient to a phosphate enema before the flexible sigmoidoscopy. ■ Fifth, these patients often have low platelet counts and deranged clotting. Personally, I place an 11mm clip on each biopsy site to avoid the need for platelet transfusions and the need to correct the INR. However, this is a personal preference and for example the ASGE recommend bringing the platelet count up to above >50 × 109/L before biopsy (>20 for an endoscopy without biopsies). ■ Sixth, consider the possibility of superimposed infection, particularly if there is superficial ulceration as both CMV and HSV causes ulceration. Biopsies for viral cultures have to be placed in viral transport medium. Of course, the ward team should also have sent stool for viral PCR (adenovirus, astrovirus, rotavirus, noro-virus can all cause watery diarrhoea) as well as for bacterial pathogens such as C.diff and C. septicum as well as for parasites such as Giardia and Cryptosporidia Recently, I've had five referrals for GVHD. All patients were on high dose steroids (eg. 80mg of prednisolone) and in none of them did it seem to make any difference to their symptoms! All of the patients felt awful with abdominal pain, profuse diarrhoea and swollen limbs (from hypoalbuminaemia). Sadly, 2 out of 5 died within weeks of their flexible sigmoidoscopy. |
Categories
All
|