|
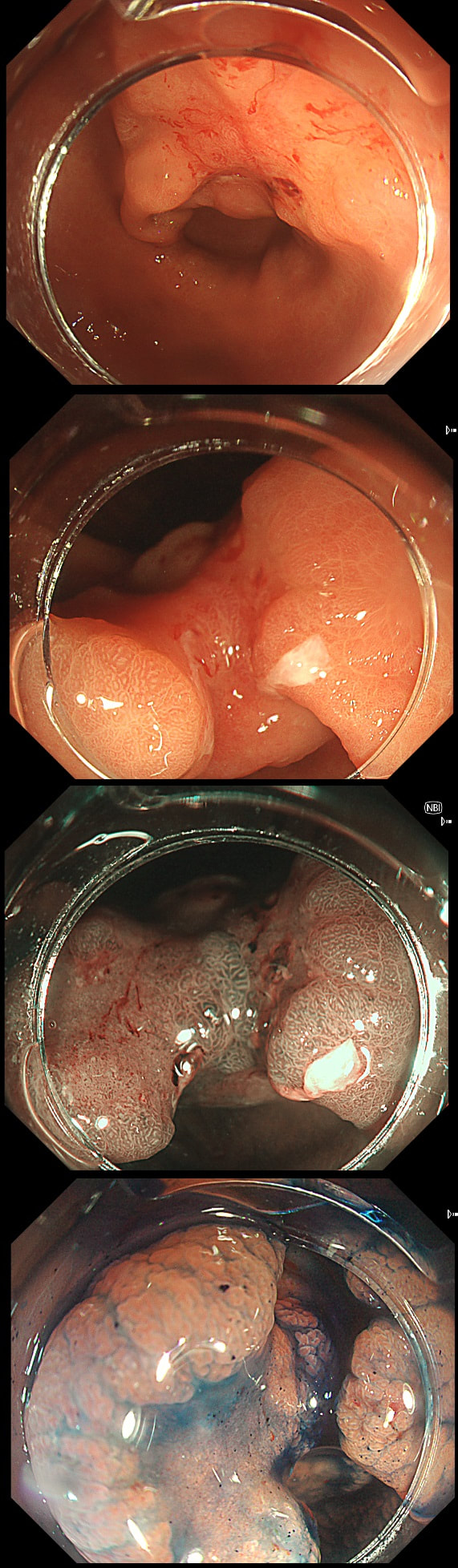
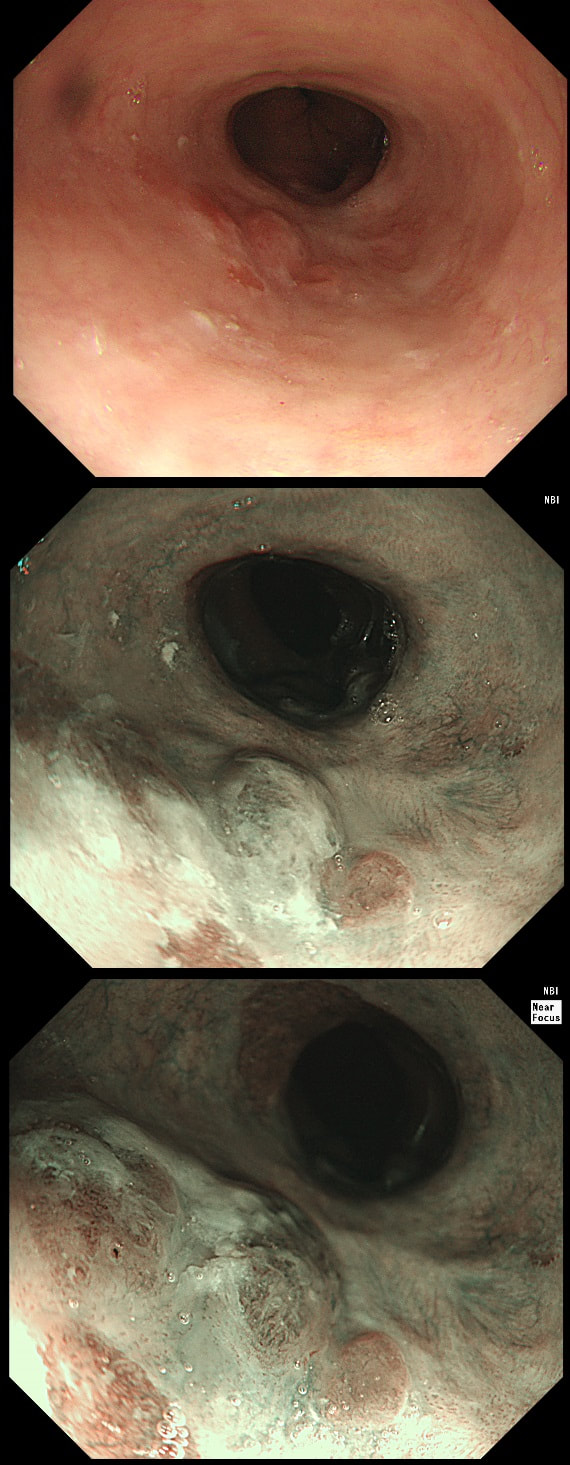
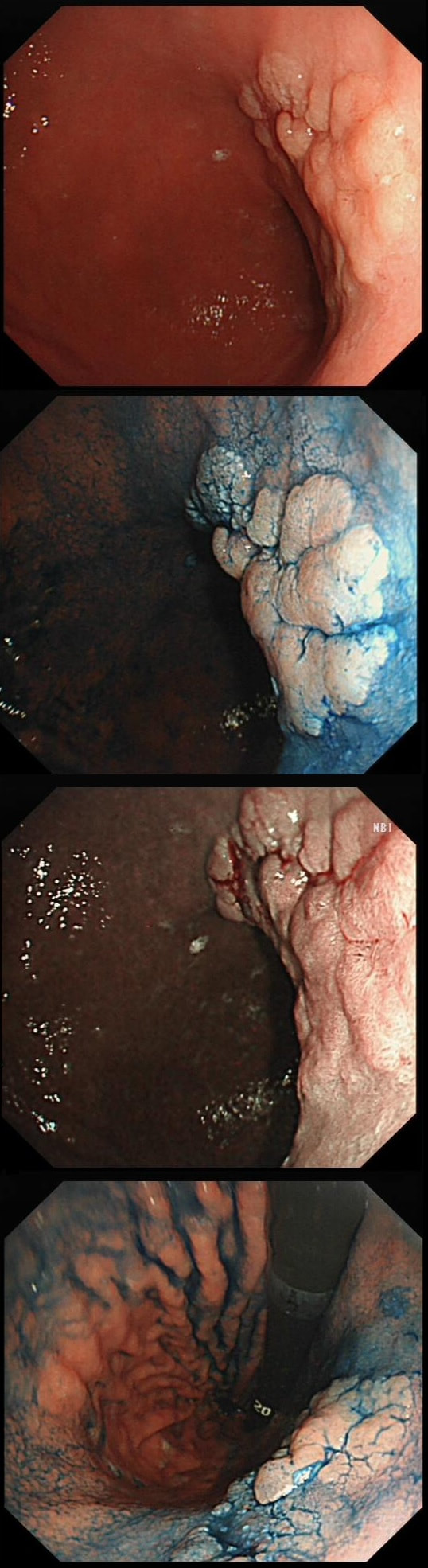
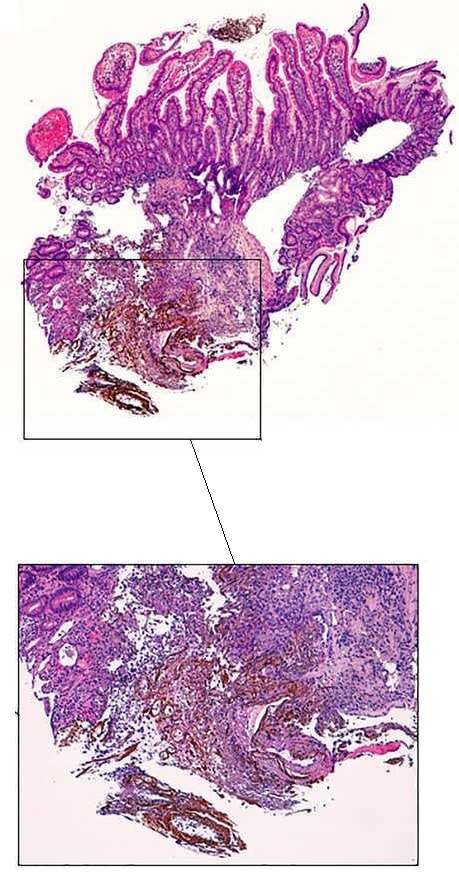
This gastric lesion is found in an 85 yr old man. Samples have confirmed a moderately differentiated gastric cancer but the lesion can't be seen on CT. The patient is frail with multiple comorbidities and declines both an endoscopic resection and surgery. However, he does ask how long it will take before he dies from the cancer?
WHAT WILL YOU ANSWER?
a) 1-2 yrs
Definitely too pessimistic!
b) 2-3 yrs
Hmm, perhaps if the lesion is poorly differentiated but it doesn't look it!
c) 3-4 yrs
This is probably how long it will before that cancer is at an advanced stage but patient will probably survive for another couple of years beyond that 'transition point'
d) 4-5 yrs
Probably too pessimistic still!
e) >5 yrs
With limited information this is the only figure backed up by some data.
Explanation
This question is something of an homage to Sir David Cox who developed the well known 'Cox Regression analysis'. Professor Cox died in 2022. As you know, the 'Cox Regression analysis' basically explores the relationship between the length of survival and more than one variable.
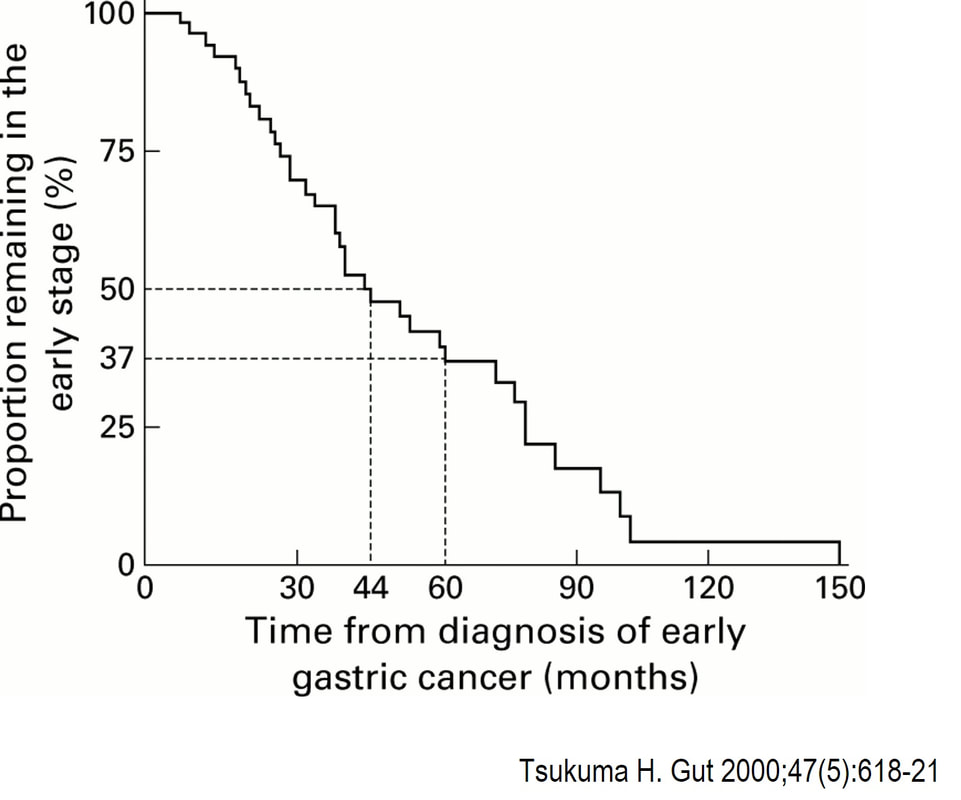
You would expect the following 'variables' to influence cancer-specific survival; histology, size of lesion, stage of lesion and perhaps the macroscopical type of early gastric cancer. Perhaps the location within the stomach also influences survival. There is some data that lesions at the gastric cardia are worse. Of course we don't have data on any of these 'variables'. However, I know of one paper by Tsukuma et al [Gut 2000;47(5):618-21] which did look at the natural history of 56 early gastric cancers in Osaka, Japan. This paper was actually a riposte to an earlier editorial from Leeds by one of my colleagues arguying that EGC is a 'pseudo-disease [Everett S. Lancet 1998;351:1350–2]. As you would expect, 56 EGC's is not enough for any sub-analysis of the above variables. Also they didn't actually look at survival. They looked at the average time it took lesion to progress from what appeared to be 'early' gastric cancer (i.e. confined to the mucosa or submucosa) as diagnosed by endoscopy. And here we reach the first issue! How sure can we be that the lesion in the image is an EGC and hasn't started to invade into the muscle propria (thus being advanced)? The lesion is about 2cm across and there is a an organised crypt pattern in the centre (can't comment on the vessel pattern as there are no magnification images). It does look 'early' and I stand at least an 80% chance of being correct in that diagnosis. Incidentally, 'lifting' is not a reliable sign in the stomach as any ulceration of the mucosa will tether it down, regardless of stage of invasion. The authors were pleased to report that if patients are left for long enough, those EGC's will grow and progress. No surprise there then! But the rate of progression was slow!!! The median time it took for 'early' gastric cancers to progress to advanced gastric cancers (i.e. T2 or worse) was estimated to be 44 months but probably shorter in patients with poorly differentiated cancers. Furthermore, the cumulative 5 year corrected survival in patients who never underwent surgery was about 63%. The answer to the question is therefore 'e'. This patient is likely to live more than 5 years from diagnosis of his early gastric cancer. Better than expected here is the Kaplan-Meyer curve below ! This patient is undergoing a gastroscopy because of dyspepsia. WHAT IS THE LIKELY DIAGNOSIS?
a) Hyperplastic polyp
It's unusual to see a ulceration on a hyperplastic polyp
b) GIST
Unlikely as the lesion isn't covered with entirely normal looking gastric mucosa
c) NET
Although there are none of the classical chunky vessels around its neck, there are other smaller nearby lesions with some unusually large vessels
d) Adenoma
Gastric adenomas are usually flat, plaque-like lesions
e) Early gastric cancer (EGC)
EGC is a good guess and patients with atrophic gastritis often do have nearby small type I gastric NET's. However, this isn't an EGC.
explanation
As you well know, gastric NET's are classified as; type I (70%-80% of gastric NET's) linked with hypergastrinaemia secondary to an atrophic gastritis and classically appearing as multiple, small gastric nodules. Then we have the rare type II gastric NET which account for about 5-8% is associated with hypergastrinaemia from a gastrin-secreting tumour such as in the MEN-1 syndrome or the Zollinger–Ellison syndrome. This was a type II gastric NET which has arisen in a patient with a pancreatic gastrinoma and MEN. Several other much smaller NET's have arisen in the nearby gastric mucosa. Finally, we have the type III NET (20%) which are solitary, large nodules with a high mitotic index arising in a healthy gastric mucosa. These are the ones not to miss as they need a cancer-like gastric resection. To remind you of the lessons from Prof Mark Pritchard's Podcast on gastric NET's, you should; AT ENDOSCOPY: • Look for atrophic gastritis • Consider using some pH indicator strips to measure the gastric pH (unless pt is taking PPI) • Identify all the NETs, record their size and number and sample them for histology and grading • Take antral and corpus biopsies and ask pathologist to do report on the presence/absence of gastric atrophy and intestinal metaplasia and also ask them to carry out immunohistochemistry stains for ‘gastrin’ in the antral biopsies and ‘chromogranin’ and ‘synaptophysin’ in the gastric body samples. • Look into the second part of the duodenum for the small submucosal gastrinomas which occasionally are seen in MEN-I • Consider samples for Coeliac disease if the patient has IDA CONSIDER OFFERING ENDOSCOPIC RESECTION FOR: • type I gastric NETs if >10-15mm • type II gastric NET if they’re causing problems (eg bleeding) and/or gastrinoma can’t be resected • type III gastric NET <1cm (provided that it's no worse grade 1/low grade 2 !) HISTOLOGY: If that proliferative index comes back surprisingly high (>10%), make sure that the pathologist hasn't inadvertently counted Ki67 positive cells in the nearby gastric mucosa. Atrophic gastric mucosa is usually more proliferative than the NETs! BLOOD TESTS: • FBC • Full haematinic screen including B12 and Ferritin of course • TFTs • Anti-parietal cell AB & Intrinsic factor AB titres • Serum gastrin level • Chromogranin level • Calcium and PTH level (particularly if MEN1 is suspected) REQUEST THE FOLLOWING SCANS FOR EVERYONE WITH LIKELY TYPE II AND III DISEASE: • CT • 68Gallium DOTA-peptide PET/CT scan • EUS to search for duodenal wall gastrinomas and small gastrinomas within the pancreas which CT can't see and to search for lymphadenopathy close to the NET
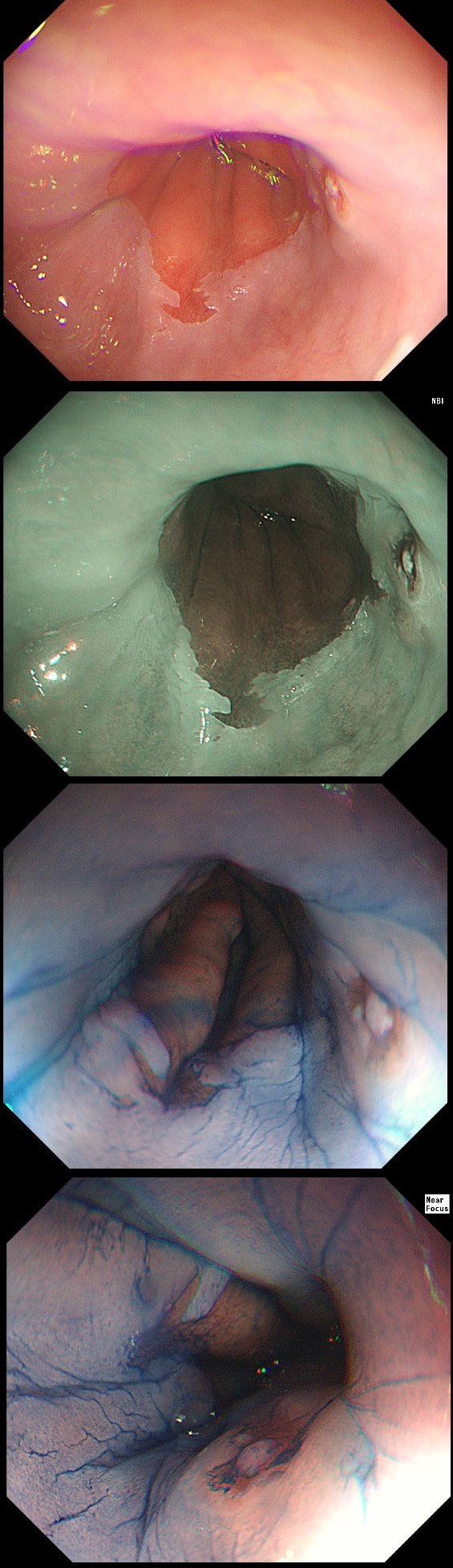
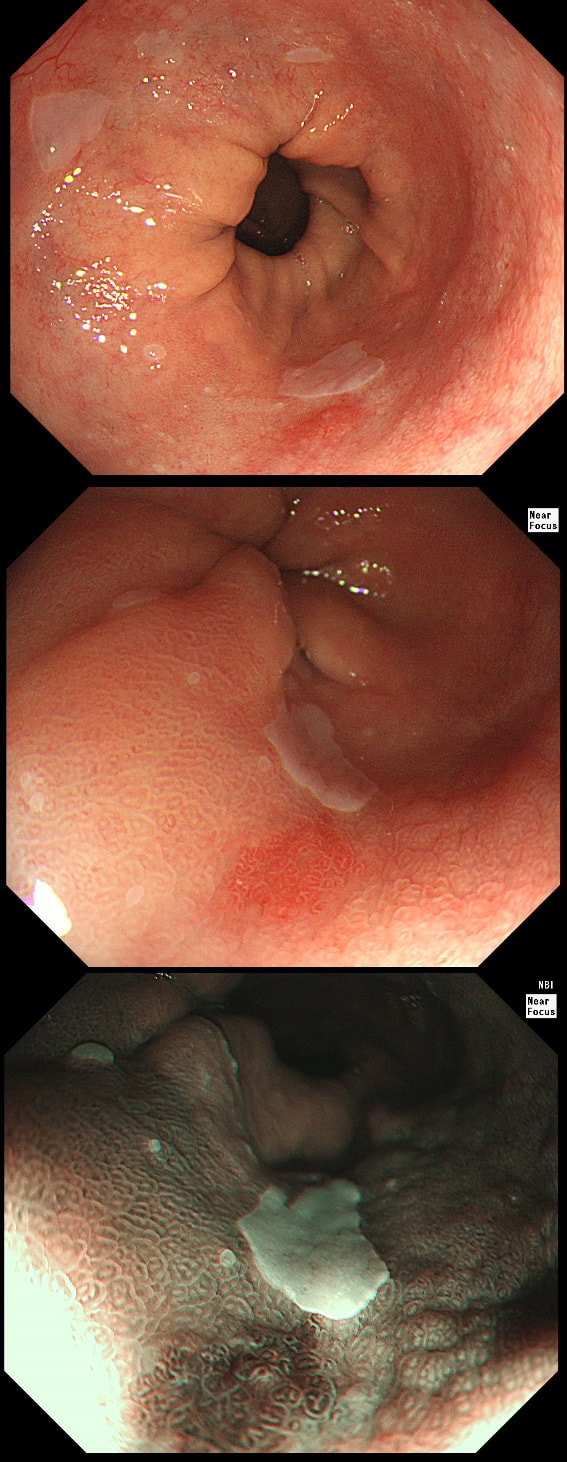
a) Reflux oesophagitis
An irregular squamo-columnar junction does suggest previous reflux oesophagitis but in this case there is more...
b) Non-dysplastic short segment Barrett's
Short-segment Barrett's is defined as Barrett's up to 3cm. In contrast, 'ultra-short Barrett's is less than 1cm. We sized the Barrett's as C0/M2 (according to the Prague classification). However, it doesn't look non-dysplastic!
c) Barrett's with intra-mucosal cancer
This would have been my own guess. There is no 'thickness' to the lesion and there is no ulceration, two features which would suggest that the lesion can't be removed endoscopically
d) Siewert II invasive cancer
Of course it may be invasive but that would be a little surprising. Endoscopically, this is IMca. Similarly HGD is unlikely as there is a lot of mucosal irregularity and you can see something has infiltrated below part of the squamous mucosa in the 2 o'clock position.
explanation
As you know, most of the time Barrett's neoplasia develops on the right-hand side and in the distal (rather than the proximal) Barrett's segment. In this case, in the 2 o'clock position there is a subtle mucosal irregularity. In fact, there appears to be something infiltrating below the squamous mucosa at this location. Biopsies had suggested IMca and a CT had been reassuring. Because the lesion is endoscopically resectable, we didn't bother with an EUS. The lesion was removed and confirmed as a poorly differentiated adenocarcinoma with signet ring morphology. On the other hand, all margins were clear and there was no LVI (lympho-vascular invasion). In the hierarchy of poor prognostic features, LVI and depth of invasion (>500µm) are the most important whilst poor differentiation is the least important. Nevertheless, I was a little worried when the patient declined surgery...
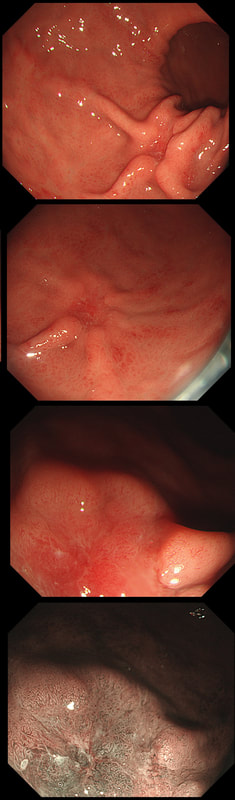
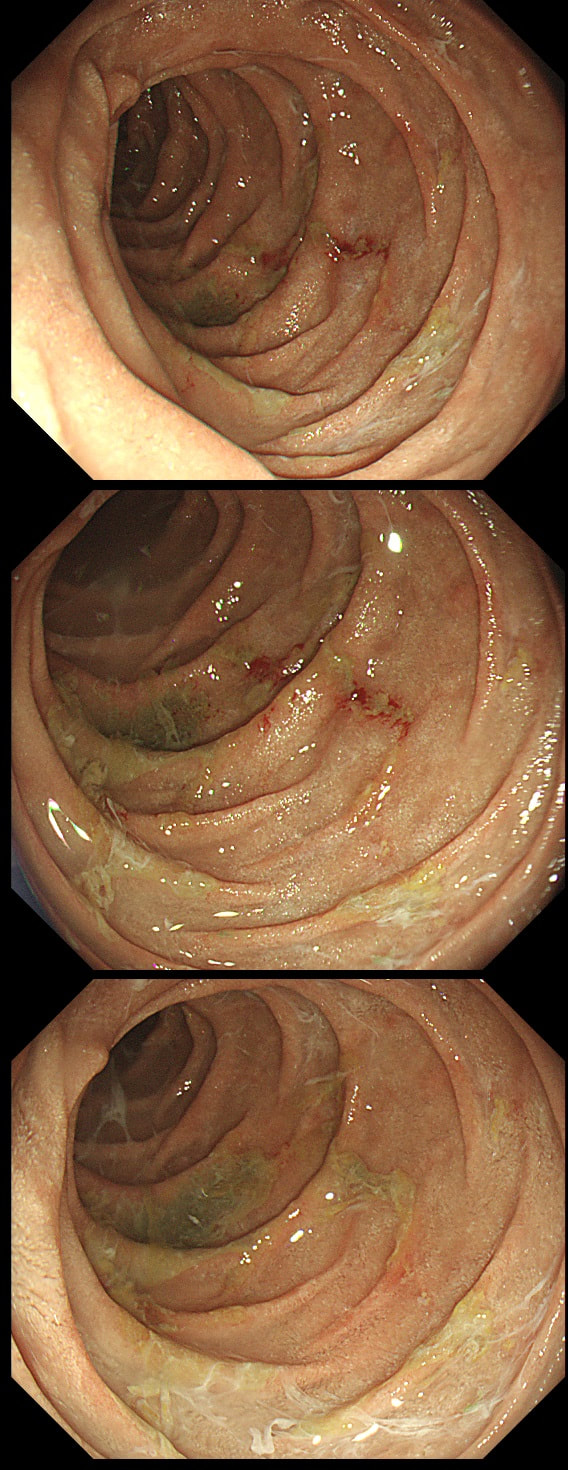
This is the stomach of a middle aged lady undergoing gastroscopy because of anaemia.
WHAT IS THE DIAGNOSIS?
a) HP associated gastritis
This is beyond gastritis! The fundal mucosa is pale and atrophic rather than red and inflammed!
b) Atrophic gastritis
The fundal mucosa does appear atrophic apart from a few scattered red patches which is all that remains of the normal gastric lining. But how about the antrum?
c) Autoimmune gastritis
Correct!
D) Coeliac disease
That duodenal mucosa is unremarkable. The 'polyp' in the 3 o'clock position is obviously the duodenal papilla.
Explanation
Those red spots in the gastric fundus is what remains of the more normal gastric mucosa whilst most of the surrounding mucosa is atrophic. In contrast, the antrum is unremarkable, as is the duodenum. This is an example of a 'body predominant' gastritis and your endoscopic diagnosis should be an autoimmune gastritis! The antral G-cells, found deep within the antral pyloric glands are pumping out huge amounts of gastric which is leading to ECL cell hyperplasia and multiple small NET's. In fact, most patients with type I gastric carcinoids have an autoimmune gastritis! The anaemia was due to vitamin B12 deficiency.
This was found in the duodenal cap of a patient undergoing gastroscopy because of dyspepsia.
APART FROM TAKING SAMPLES, WHAT ELSE SHOULD BE DONE?
a) take a CLO test
Absolutely correct!
b) take gastric biopsies
Will show a Hp associated gastritis
c) take samples from D2
That's a no from me...
d) request an EUS
Never seem to be the right answer!?
e) request a CT
Perhaps if bx against all odds with suggest lymphoma but that would be a long shot
explanation
You first guesses when you find funny bumps in the duodenal cap should be gastric metaplasia and gastric heterotopia. Brunner's gland hyperplasia is also common but are never multiple (at least I have never seen a case with more than one nodule from Brunner's gland hyperplasia).
This is a case of foveolar gastric metaplasia in the duodenal cap. Basically, the mucosa in the duodenal cap has become more 'stomach-like' with crypts lined by mucus secreting cells (foveolar cells) which are different to goblet cells found elsewhere in the GI tract. Gastric metaplasia is common in patients with a history of peptic ulcer disease and is thought to be a defence response or adaption to the presence of excess acid in the duodenum. It's thought that Helicobacter are able to colonise the foveolar gastric metaplasia in the duodenum and this contributes to duodenitis and duodenal ulceration. So, what should you do next? Do a CLO test for Helicobacters of course!
A somewhat scary dilatation.
WHAT IS THE LIKELY AETIOLOGY OF THE STRICTURE?
a) peptic stricture
There are no linear reflux ulcers!
b) eosinophilic oesophagitis
yes! Long and fusiform stricture and mucosa 'splits' in a frightening way
c) SCC
Those IPCL's do look a little prominent but not ectatic etc
d) adenocarcinoma
But the stricture is within the squamous part of the oesophagus!
explanation
Eosinophilic oesophagitis was first described in 1978 and is widely regarded as an allergic condition. Food allergy may play a significant role and the majority of sufferers have either personal or family history of other allergic conditions.
In contrast, Lymphocytic oesophagitis is much more recent, first described by Rubio et al in Sweden in 2006. As yet there is no consensus on how many lymphocytes are needed to make the diagnosis. Extrapolating from EoE, I take 2 samples from the proximal, middle and distal oesophagus respectively, in all patients with inexplicable dysphagia. LyC oesophagitis is still regarded as something of an entity "in search of a disease". For this reason it's difficult to know if the reported increasing prevalence is simply due to the pathologists being on the lookout and more oesophageal samples (correctly) being taken in patients with dysphagia. There is an association with old age, female gender, smoking, reflux disease and primary esophageal motility disorders. Clinically oesophageal rings, webs, nodularities, furrows and strictures have been described in both conditions. Personally, I think that they look subtly different! I suggest a LyC oesophagitis when there is subtle dilatation of the intrapapillary capillary loops within the squamous oesophagus. In my experience you don't usually see this in EoE. For this reason, a lymphocytic oesophagitis would have been a very reasonable guess in this case. Those IPCL's do look a little dilated don't they? Of course, strictures are supposedly far less common in LyC oesophagitis than in EoE.
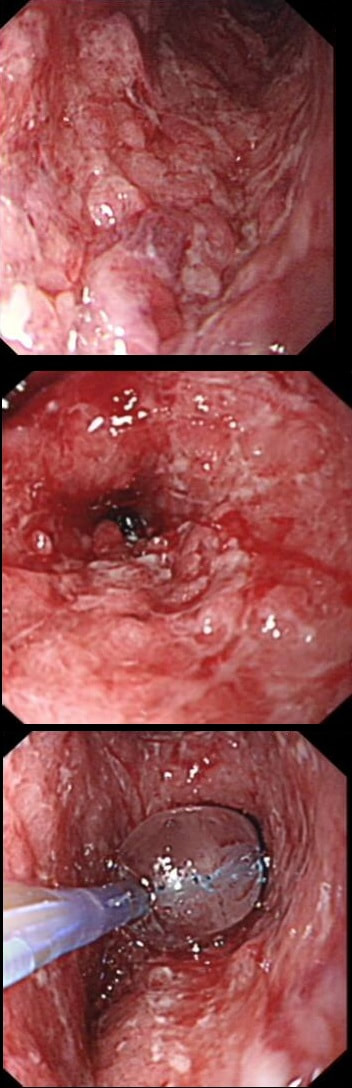
Patient with Barrett's harbouring HGD has been treated with RFA. He has now returned for the second RFA session when this is found.
WHAT IS YOUR ENDOSCOPIC DIAGNOSIS?
a) Benign scarring
Doesn't look benign - Looks evil!
b) Local recurrence of non-dysplastic Barrett's
Barrett's are re-emerging in several places. Doesn't look benign!
c) Barrett's adenocarcinoma
Absolutely! Nodules are never allowed in Barrett's!
explanation
Actually, there is a re-emergence of several brown nodules below the squamous mucosa. Biopsies confirmed this as an invasive adenocarcinoma, re-emerging from below the 'neo-squamous mucosa'. Clearly, to try RFA again would be a mistake! The histology showed a 'poorly differentiated' cancer and we are recommending either surgery or chemo-radiotherapy next (CRT). Even if histology hadn't shown poor differentiation, this 'smells' like bad disease to me which we may well 'undertreat' endoscopically.
WHAT IS THE MOST LIKELY DIAGNOSIS?
a) Portal hypertensive gastropathy
Doesn't really look like 'snake skin' does it?
b) HP associated gastritis
HPAG is a great mimicker but not this time
c) Gastric vascular ectasia
Absolutely, affecting the whole stomach!
d) Lymphocytic gastritis
LyC gastritis is ulcerative!
e) Linitis plastica
Another great mimicker but this is a vascular issue rather than mucosal infiltration!
explanation
Of course, this is a case of Gastric Vascular Ectasia. As the whole of the stomach is affected, I don't think that we can call it 'antral' ectasia. Gastric antral vascular ectasia “GAVE” (watermelon stomach) has been described with; • Cirrhosis • Atrophic gastritis/achlorhydria/hypergastrinaemia • Connective tissue diseases (especially systemic sclerosis and hypothyroidism) • Diabetes • Heart failure • Chronic renal failure It has been proposed that the underlying link between all the different conditions associated with GAVE may have autonomic dysfunction in common leading to prolapse of the antral mucosa through the pylorus. Must admit that I'm sceptical! A study suggested that a “punctuate pattern”, as seen in this clip, is typical of cirrhosis whilst a “striped type” was more common in non-cirrhotic cases. Indeed this patient had NASH cirrhosis. Portal hypertensive gastropathy probably has a different aetiology and is a different condition as gastric antral vascular ectasia can develop with a normal portal pressure. Patients with vascular ectasia of course usually present with iron deficiency anaemia. Patients with bleeding from GAVE were previously treated with antrectomy. Now, the first line treatment is “thermal therapy”. Octeotride and oestrogen-progesterone have also been used in small series but would now only be considered if endoscopic therapy fails. It is far easier to treat these lesions using the argon coagulator than the heater probe. Using a banding device may be quicker in patients who tolerate gastroscopies poorly. RFA is also effective but is VERY expensive. This patient attends for Barrett's surveillance WHAT IS YOUR DIAGNOSIS?
a) Barrett's without dysplasia
A nodule within Barrett's is NEVER 'normal'!
b) LGD
LGD is flat, not nodular!
c) HGD
Good guess! Although your guess actually proved to be wrong
d) IMca
Small crypts + nodule = correct!
e) invasive cancer
Nodule should have been larger and without those small crypt openings
explanation
My 'rules of thumb' when assessing Barrett's is as follows: 1) crypts look different in a distinct patch but the area is flat = LGD 2) areas of superficial ulcers within the Barrett's = widespread LGD 3) crypts look different and there is a distinct nodule = HGD 4) crypts are tiny small and there is a nodule = IMca 5) there are no crypts and there is larger nodule = invasive cancer Of course this isn't fool proof ! After all, it's very difficult to distinguish HGD from IMca even on histology! However, it gives you a starting point on how to assess Barrett's and what you should enter on that Histopathology request form. Remember that your pathologists need your help! This lesion was found at gastroscopy WHAT IS YOUR ENDOSCOPIC DIAGNOSIS?
a) Siewert I SCC
Nope!
b) Siewert I adenocarcinoma
Lesion isn't centred 1-5cm above the GOJ
c) Siewert II adenocarcinoma
Yes! Lesion staged as T2,N0 on PET-CT
d) Siewert III adenocarcinoma
Lesion isn't centred 2-5cm below the GOJ
explanation
This lesion is clearly malignant with a rolled edge and surrounding mucosal ulceration. It was confirmed as a Siewert II adenocarcinoma, T2,N0. Cancers at this location are becoming more common. They are easy to miss, particularly if you don't slow down as you traverse the gastro-oesophageal junction (GOJ) and/or retrovert at a distance. On retrovertion you need to pull the scope back up so that you can have a close view of the cardia. Siewert et.al. developed the classification as follows:
Of course it can be difficult to determine where the epicentre of a cancer is, particularly on imaging. At endoscopy you are in a unique position to accurately record the correct Siewert type of the cancer. It makes a difference because the Siewert type has implication for treatment! Siewert I lesions are treated with oesophagectomy and gastrectomy as these lesions usually metastasise to nodes in the mediastinum. Siewert II are 'true' junctional cancers and mainly metastasise to nodes in the abdominal nodes but in around 15-20% of cases, there are mediastinal nodes. For this reason, patients with Siewert II lesions are only offered gastroectomy (without oesophagectomy) IF there is no mediastinal lymphadenopathy. Arguably, any borderline mediastinal nodes should probably be sampled before or during surgery before a final decision is made not to clear the mediastinal nodes with the resection specimen. Patients with Siewert III cancers are usually offered total gastrectomy plus a distal esophagectomy (to get clear resection margins, a so called R0 resection ) as these lesions spread to peritoneal nodes. WHERE IS THE BARRETT'S CANCER?
a) 12 O'clock
Eagle eye!
b) 3 O'clock
But the round crypt openings say otherwise!
c) 6 O'clock
Nope!
d) 9 O'clock
Where there is hardly any Barrett's?!
explanation
Of course the lesion is situated at 12 O'clock. There you can see a subtle mucosal nodularity with an irregular vessel pattern. It was removed by 'suck within the cap' EMR and confirmed as an IMca. This lesion is being removed from the distal oesophagus WHAT IS THE LIKELY HISTOLOGY?
a) Hyperplastic polyp
You must be joking!
b) Adenomatous polyp
A gastric adenomatous polyp would surely now be malignant
c) Early malignant polyp
But it's arising from a malignant flat component!!!
d) Advanced gastric cancer
Absolutely!
explanation
Of course this is all very odd. Clearly this is an advanced cancer at the GOJ. What business do I have in 'attacking' this endoscopically?! Actually, the elderly patient had completed a course of chemoradiotherapy (CRT) for a T2, N0 junctional adenocarcinoma some 30 months previously. Now he has developed dysphagia and a CT confirmed a 2cm polyp at the gastro-oesophageal junction. Histology had shown 'at least IMca' and he was referred for consideration of an endoscopic resection. Clearly this lesion can't be cured endoscopically. In fact, the elderly patient is not a candidate for surgery and therefore there is no cure at all. However, I was thinking that as the cancer is mainly polypoidal, perhaps if the nodule could be removed, his swallowing will improve and he will not need a stent and could be offered brachytherapy. Clearly this was all 'speculative' but I'm glad to say that 6 months later, the patient still has not developed any dysphagia and his now starting brachytherapy. No doubt a better outcome than could be offered by a stent? This is a solitary gastric polyp WHAT IS YOUR ENDOSCOPIC DIAGNOSIS?
a) Hyperplastic polyp
Spot on!
b) Hamartomatous polyp
A bold guess but wrong!
c) Cystic fundic polyp
Too red and should be several of them!
d) Adenomatous polyp
But there is no defined crypt pattern?!
e) Malignant polyp
May be a 5% chance that you are right!
explanation
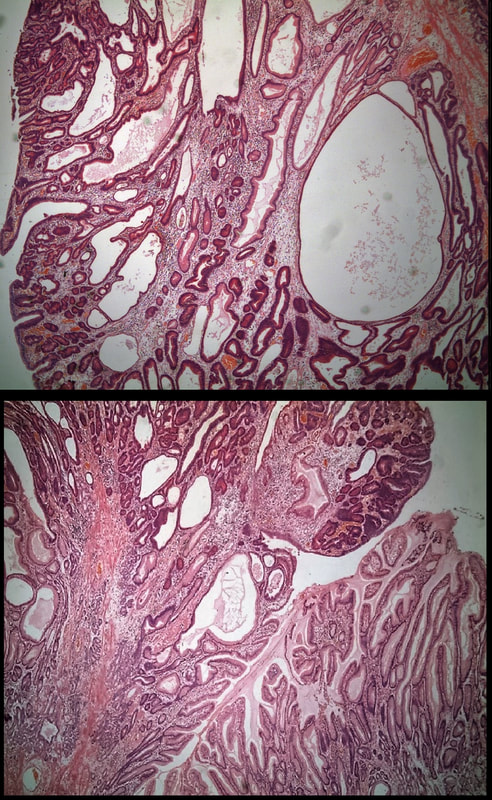
A missing piece of information, which I perhaps should have provided, was the H.pylori status of this patient! This lesion was arising from a H.pylori associated gastritis.
Most polyps found in a stomach with Helicobacter pylori associated gastritis are hyperplastic (inflammatory). They appear angrily red (because they have lots of capillaries) and often with white fibrin caps, making them look a little like mushrooms. A small proportion of hyperplastic looking polyps are actually malignant. In my experience, these 'stealth cancers' are most common close to the gastric cardia and are always solitary. Conversely, multiple inflammatory polyps in the antrum and gastric body are almost certainly benign. Of course, this is a 'solitary' hyperplastic polyp, close to the fundus. Perhaps not unexpectedly it harboured some (low grade) dysplasia (histology below). The dysplasia is in the crypts lined by deep purple/blue cells rather than the normal light pink cells. The contrast is probably best seen in the second histological slide where the dysplastic part is towards the top of the slide and the non-dysplastic is at the bottom half. If the H.pylori test is negative, and particularly if the patient is taking a PPI, the polyp is more likely to be a 'Fundic gland polyp' (cystic fundic polyp) which are full of cystic spaces and therefore look a little translucent like frog-spawn. Rarely polyps are hamartomatous as in Peutz-Jeghers polyps and the polyps arising in patients with 'Cronkhite-Canada syndrome or in Juvenile polyposis. In many cases these lesions have an odd but distinct surface crypt pattern or, alternatively look again look translucent like frogspawn. It's rather difficult to explain the appearance of a hamartomatous polyp and for this reason, I have attached some images below (after the histology slides). Another polyp, most likely to arise in an atrophic gastritis with patches of intestinal metaplasia, is an adenomatous polyp of the 'intestinal type'. To remind you, there are at least 4 types of gastric adenomas which all have an organised and regular surface crypt pattern:
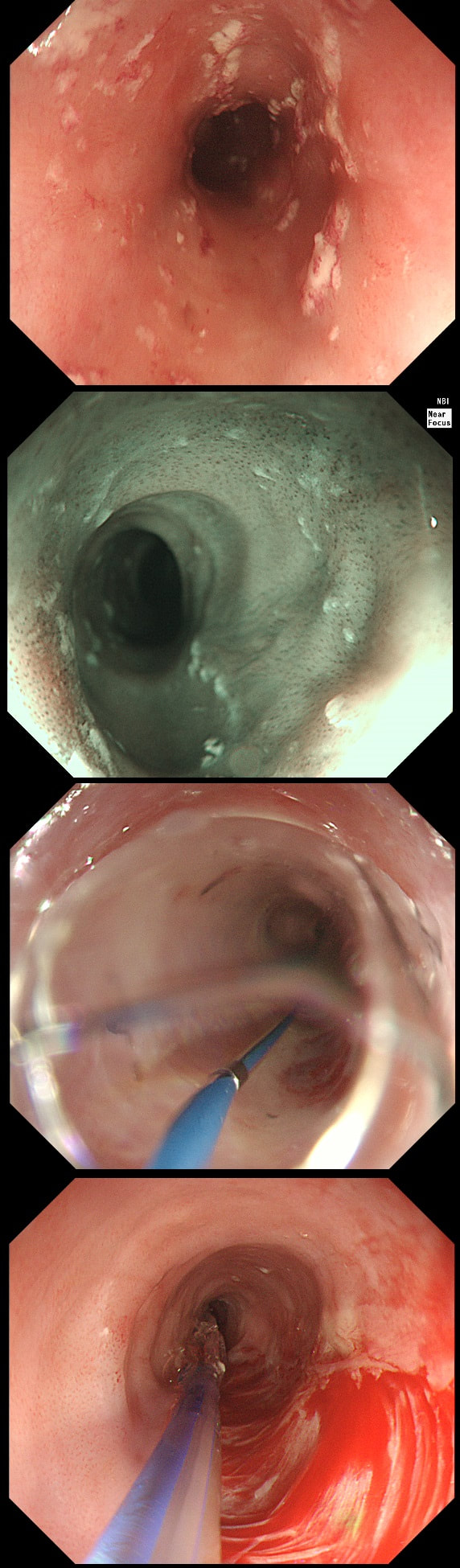
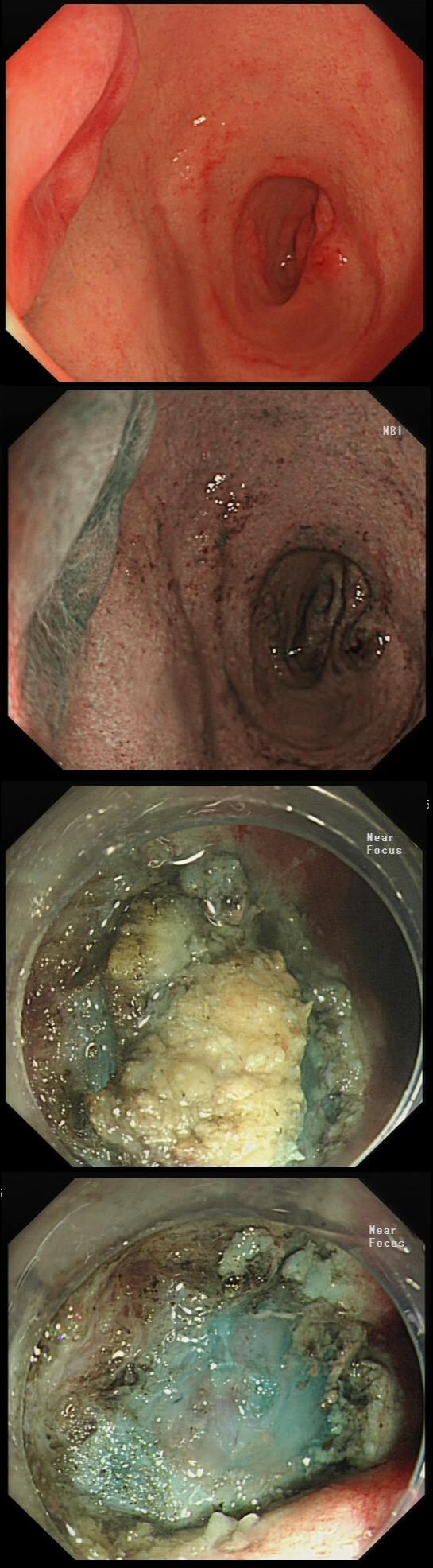
Patient was complaining of indigestion and reflux symptoms.
WHAT IS YOUR DIAGNOSIS?
a) Normal oesophagus
Not quite normal is it?
b) Reflux oesophagitis
This doesn't look like reflux!
c) Adenocarcinoma
Actually the correct answer!
d) SCC
Red nodules, even if surrounding by squamous mucosa are adenocarcinomas (usually)
explanation
You may be surprised to hear that the small nodule at 3 O'clock turned out to be an IMca! It was removed endoscopically. Of course, it's the question then arises; "Should we offer RFA". The BSG recommends this for patients with Barrett's harbouring flat dysplasia. However, in this case there is only a tiny, tongue of Barrett's in the 6 O'clock position! Actually, we just gave this a quick blast of APC (at a fraction of the cost of RFA) and it was gone. However, the patient remains on annual surveillance!
A 21-year-old man presents with a past history of intermittent abdominal pains. For the last year he has suffered with more frequently bouts of abdominal pains and more recently he has started to vomit some 30 minutes after eating. He has been started on lansoprazole for a couple of months with no response. At gastroscopy (photograph) there is a severe gastritis and a tight pylorus requiring dilatation to examine the duodenum (which was unremarkable).
His blood results are as follows: Hb 11.2 g/l MCV 105 fl WCC 11.9 x 109 Plat 395 x 109 Basal gastrin 180 pg/ml (<75) WHAT IS THE MOST LIKELY DIAGNOSIS?
a) Hp associated gastritis
Doesn't explain all the 'issues' !
b) Zollinger-Ellison syndrome
There is a simple explanation to that elevated gastrin level!
c) Crohn's disease
Well done!
d) Gastric lymphoma
The antrum would do but how do you explain the macrocytosis?
e) Diffuse type gastric cancer
Could look like this but he is a bit young isn't he? !
explanation
Although the patient has a raised gastric level, this can be explained by the lanzoprazole. The macrocytosis is more difficult to explain. An autoimmune gastritis would be expected to be worse in the gastric body than in the antrum. In fact, the only other possibility is that the patient has terminal ileal Crohn's disease, causing malabsorption of B12 as well as a Crohn's gastritis. This was indeed the case! Actually, the diagnosis had already been confirmed by antral biopsies before I carried out the dilatation! Wouldn't like to dilate a diffuse type cancer !
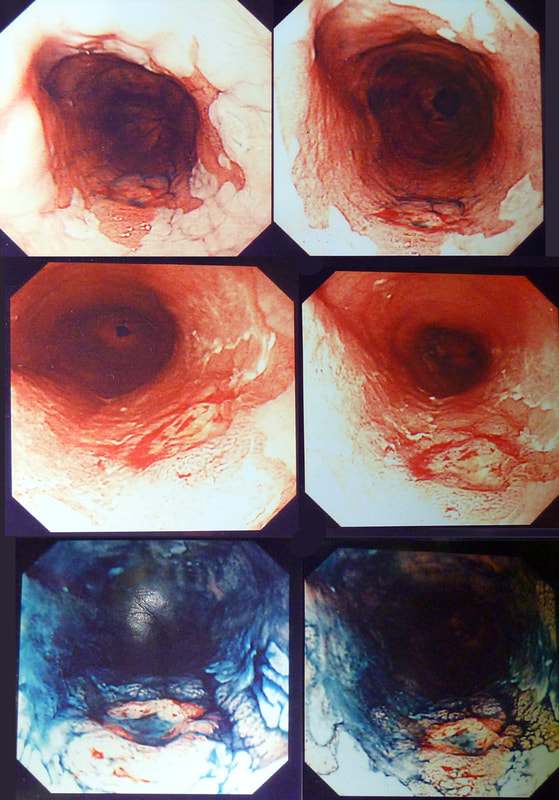
An odd lesion in the middle of the oesophagus of a 55 year old woman. WHICH OF THESE POSSIBILITIES IS THE MOST LIKELY?
a) Papilloma
Papillomas look more warty and I've never seen them ulcerate
b) Leiomyoma
Statistically the most likely benign lesion probably!
c) GIST
Are very rare in the oesophagus!!!
d) NET
Are also very rare in the oesophagus!
e) SCC
Not likely as the IPCL's are regular and the lesion isn't brownish!
explanation
GIST's are extremely rare in the oesophagus whilst common in the stomach. In contrast, leiomyomas are common in the oesophagus and rare in the stomach. However, this looks odd and the previous biopsies had not been able to get to the bottom of the diagnosis. Are we missing a SCC? However, it looks like something from deeper layers were breaking through the mucosal surface. In contrast an SCC should start growing at the surface and in time invade deeper. The 'intrapapillary capillary loops (IPCL's) dilate up, become irregular and eventually completely disorganised in SCC's. At the same time the oesophageal wall takes on a brownish tint on NBI.
I decided to remove it and it turned out to be a leiomyoma. I presume that it had got traumatised or perhaps by pressure necrosis ended up with a funny surface. Don't think that I have seen an oesophageal NET as yet. Presumably they are very rare in this location. By the way, I've uploaded an example of a T2 mid-oesophageal SCC in the clip below. The lesion looks smallish but is already beyond endoscopic cure and Lugol's shows up a large area of background dysplasia which looks orange rather than brown after Lugol's dye spray.
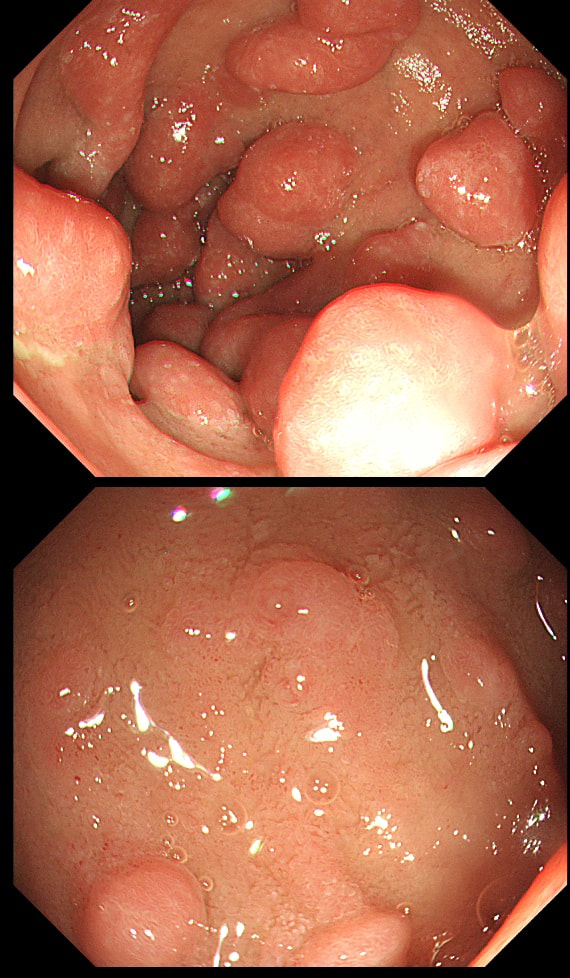
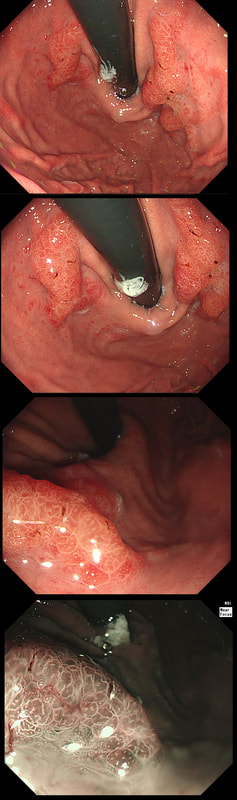
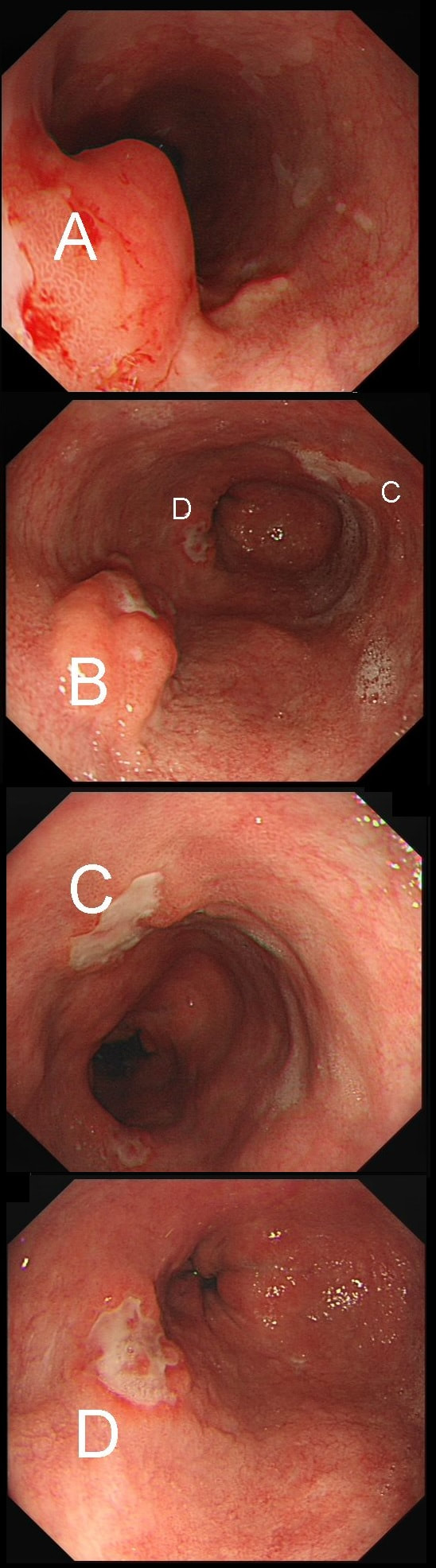
55 yr pt with a Barrett's nodule is referred for an endoscopic resection. I'm surprised to find 4 abnormalities within his 10cm stretch of Barrett's
WHICH OF THESE IS THE MOST LIKELY TO BE ENDOSCOPICALLY RESECTABLE?
a) Lesion A
I agree! Of these 4, A is the only one which isn't ulcerated and therefore is least likely to be invading deeply.
b) Lesion B
Would be my second guess as the ulcerated area seem superficial
c) Lesion C
Don't like the ulceration!
d) Lesion D
Would be my least favourite lesion to attack as the ulceration suggests deeper invasion and poor lift into my cap.
explanation
This may be something of a record, 4 synchronous lesions! Clearly A, B and D are malignant. At first, ulcer C seem more innocent without an elevated edge but on closer assessment, it also has a slightly elevated rim.
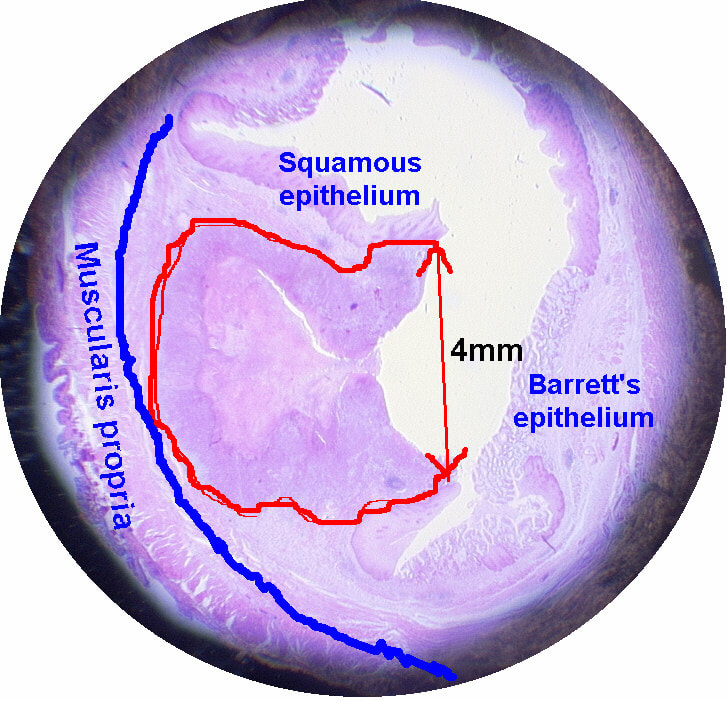
Of these 4, A is the only one which isn't ulcerated and therefore is least likely to be invading deeply. Of course, they are assessed together as there is no point in EMR'ing one only. Either all are curable endoscopic means or none are ! Rather than going ahead with attempting to resect these, I actually bailed out and took samples from each lesion. Biopsies showed invasive, poorly differentiated adenocarcinoma at each location! Clearly, this patient has multifocal 'bad disease' which endoscopy is unlikely to cure in my opinion. I believe that surgery is a far better option and the patient is currently awaiting his oesophagectomy. If you still are not convinced of the pitfalls in trying to deal with ulcerated Barrett's lesions, have a look at the lesion below. Two rounds of sampling had indicated that the lesion harboured HGD. However, I failed to remove the lesion and ultimately the patient underwent an 'Ivor-Lewis'. You can see the histology yourself. The 4mm surface is literally the tip of the iceberg and below you can see the cancer (red line) invading up to the muscle propria.
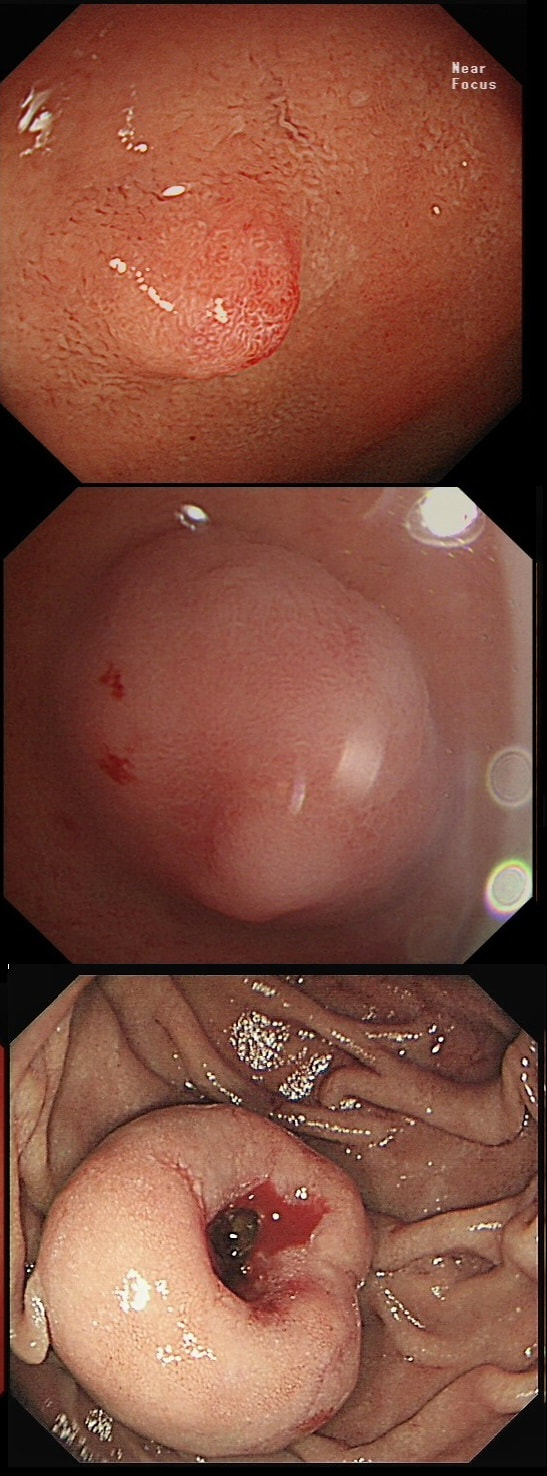
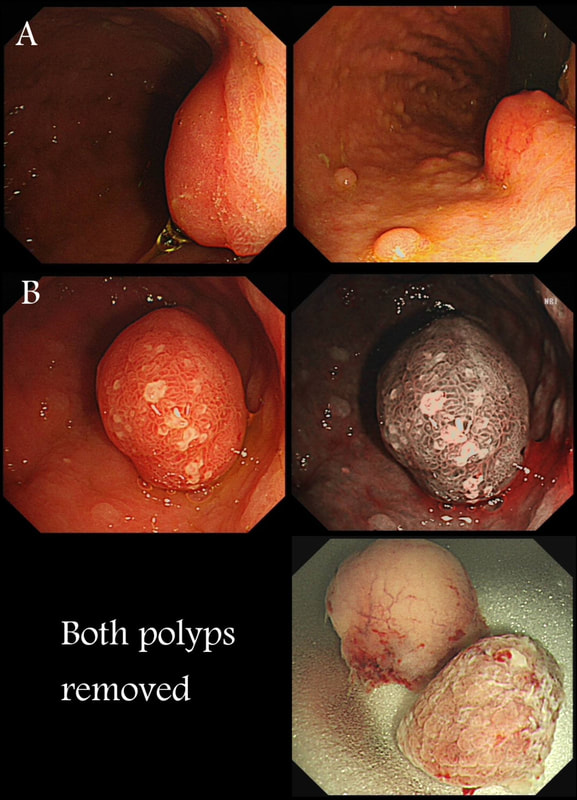
This polyp found on the lesser gastric curve.
WHAT IS THE MOST LIKELY DIAGNOSIS?
a) Hyperplastic polyp
HP polyps are usually subpedunculated and angry red
b) Intestinal metaplasia
IM is also 'pale' but not 'flat elevated'
c) Gastric adenoma
Would be my first guess!
d) Early invasive cancer
This is a plaque without a depression or dominant nodule to suggest invasive cancer
explanation
Of course, this could have been rather easy to miss! An insignificant pale, plaque-like lesion but with distinct borders best seen after indigo carmine dye spray (as usual). Endoscopically this is what a gastric adenoma looks like and it was removed endoscopically. Somewhat surprisingly, histology reported a small spot of IMca and therefore its at actually an early cancer - not invasive though!
Most invasive, gastric EGC's are of course shallow depressions as in the example below. In fact the lesion below was invading into the middle of submucosa and was confirmed as poorly differentiated. Afterwards the patient underwent a distal gastrectomy where no further cancer was found. 'Poor differentiation' is the least reliable and lymphovascular invasion (LVI) is the most reliable predictor of nearby lymphnode micro-metastases.
This lesion was referred for resection just beyond the pyloric ring. It seemed to lift well but rather to my surprise, the snare cut through the base of the lesion (bottom image on the left). It took some further lift and a stiff snare to scrape the lesion of the muscle propria layer.
WHAT IS THE LIKELY HISTOLOGY?
■ Adenoma
Adenomas are usually not umbilicated ...
■ Brunners gland hyperplasia
I don't bother to remove those and they are not umbilicated!
■ Gastric heterotopia
Is usually found at this location but never require EMR
■ NET
Of course it is - it's umbilicated !!!
■ Early malignancy
Would be VERY rare in the duodenal cap!
explanation
The lesion is umbilicated... As you probably remember, umbilicated lesions in the duodenum are usually NET's. For some reason, they look different to NET's found elsewhere in the gut, where thin vessels are usually seen crawling up their sides. In the photograph below, you can see that at the very earliest stage (first image), there is no central indentation. However, very soon a subtle central dip develops (second image) which at the advanced stage (when I was tasked with removing the lesion), it has a deep central pit which was intermittently bleeding.
This proved to be a WHO grade I NET (neuroendocrine tumour, with a mitotic rate <2%). These lesions always seem to be tethered down close to the muscle propria and can be difficult to remove without taking a chunk of muscle propria with it. Duodenal NET's should of course be discussed at the 'neuroendocrine MDT' and usually end up having: 1) Measurement of plasma chromogranin A (pCgA) levels. CgA is produced by all cells derived from the neural crest and high levels are found particularly in patients with metastatic disease. 2) A ‘gut hormone screen’ (measurement of gastrin, glucagon, vasointestinal peptide, somatostatin and pancreatic polypeptide levels). 3) Finally, an ‘octreotide scan’ (somatostatin receptor scintigraphy) or, even better, a PET/CT scan using peptides that bind to somatostatin receptors (68Gallium-DOTA-TOC/NOC/TATE).
This was found on the anterior gastric wall in an elderly patient with iron deficiency anaemia
WHAT IS THE MOST LIKELY DIAGNOSIS?
■ Gastric ulcer scar
Quite possible but you would take samples surely?
■ Gastric erosion
But there is a nodule in the centre?
■ Benign gastric ulcer
But there is no 'ulcer' in the centre?!
■ Early gastric cancer
Surely, the most likely diagnosis?
explanation
Gastric folds are being pulled into this 'lesion'. Of course most EGC's are depressed or flat elevated with a central depression. This is not easy to classify into the Paris classification system. I guess that you can argue that its' an elevated lesion with a central depression? Anyway, at the centre of the lesion there is a nodule! Not an ulcer! It's most likely an EGC. In fact, the lesion was resected endoscopically and proved to be poorly differentiated invasive cancer with a positive deep margin ! As the patient was 84 yrs old, no surgery was offered. That was 6 years ago and the patient remains well with only an unremarkable scar in the stomach to remind him ! Wonderful !
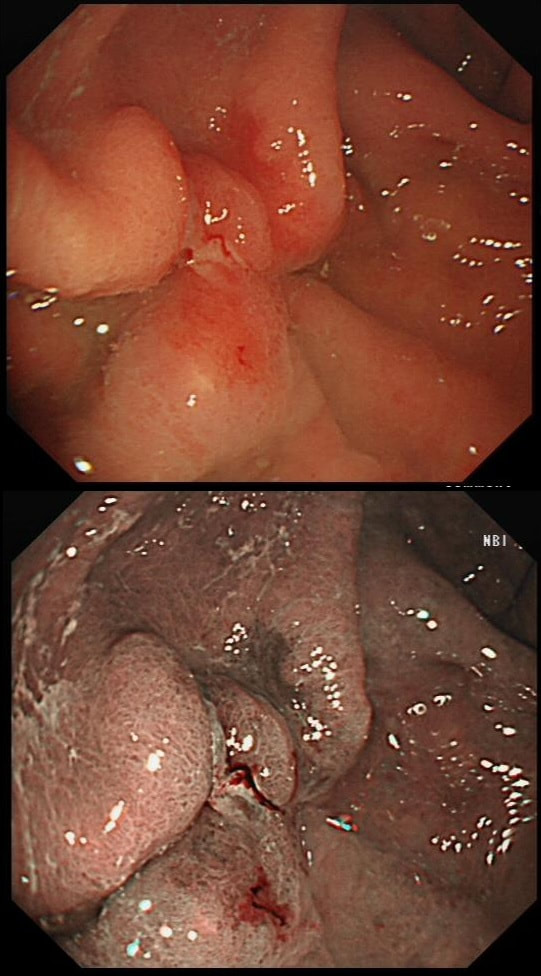
Two gastric polyps (labelled A & B) were both removed from the stomach of a 60 year old woman who complained of indigestion.
WHAT IS THE LIKELY DIAGNOSIS?
■ Both are hyperplastic
But the look different to each other!
■ NET + HP polyp
Well done ! And presumably you know which is which?
■ Both are NET's
But they look different!
■ HP + Adenoma
How about those fine vessels seen in the second image?
■ Both are adenomatous
But they look different!
explanation
You can see the thin vessels crawling up the side of polyp A. This appearance is typical of a gastric NET. Polyp B has a more villous surface with a few white spots - all typical of a hyperplastic gastric polyp. Some of these may contain some malignant cells which somehow generate a hyperplastic/reactive/inflammatory reaction around themselves. However, most hyperplastic gastric polyps are benign and arise secondary to a Helicobacter pylori gastritis. For this reason, you should always do a CLO test in these cases.
Every few weeks, I look up the notes on Prof Pritchard's' Podcast on gastric NET's to remind myself of the workup of these cases. As you remember, you should take samples to confirm an atrophic gastritis whenever you find a gastric NET. In this case, the patient did NOT have an atrophic gastritis. Instead, there was a Hp associated gastritis which is the reason for the second polyp. We realised that what we had was a TYPE II gastric NET! Analysis confirmed that the 17mm was WHO grade II. The finding of anything else than an innocent Type I gastric NET means that further imaging was required. A little late in the day of course but fortunately, the following imaging investigations were unremarkable:
Anyway, below is a reminder of what to do at gastroscopy, when you have a case of gastric NET:
This patient attended for dilatation of his biopsy confirmed peptic oesophageal stricture. Clip has been speeded up somewhat. WHAT WOULD YOU ORGANISE NEXT?
■ A clinic appointment
To ask pt about the swallowing? Hmm, somethings missing!
■ Another dilatation in 2 weeks time
Stricture not very tight and the dilatation should last longer
■ an early follow up OGD for biopsies
The mid-oesophageal stricture is peptic but what of the mucosa below?
explanation
The background to this case is a recent audit which we did in Leeds on missed upper GI neoplasia. We have had several instances of oesophageal cancers being missed when the endoscopist focused too much on the 'task in hand'. For example, we have had several SCC's missed when the endoscopist was carrying out a Barrett's surveillance endoscopy. This is another example of a missed (intramucosal) adenocarcinoma, glimpsed about 10 seconds into the clip in the 3 O'clock position. With mid-oesophageal peptic strictures there is often a stretch of Barrett's below which of course must be assessed and sampled at the earliest convenience. Of course, one can argue that when the job is to do something therapeutic, such as placing a PEG or removing a large polyp, it is 'permissible' to miss a cancer elsewhere. After all, the objective is not to undertake a careful diagnostic examination but to 'do a job'! I'm a strong believer that 'diagnostic' examinations and 'therapeutic' examinations must be clearly separated when you are looking at 'missed lesions. There is a distinct 'therapeutic window' during all endoscopic procedures done without a general anaesthetic. In the upper GI tract, it's up to 20-30 minutes and in the colon I think that it's up to 45-60 minutes. Your patient will not thank you for wasting the valuable minutes of your therapeutic window on carrying out a full diagnostic examination. Of course, after your therapeutic procedure you should consider if an early diagnostic gastroscopy or colonoscopy is needed. But carrying out a full assessment of the squamous portion of the oesophagus at the time of a Barrett's surveillance examination doesn't add much to the procedure. Similarly, when a mid-oesophageal peptic stricture is found, one should realise that the reason that the peptic stricture is in the middle of the oesophagus and not the gastro-oesophageal junction, is probably that there is a a Barrett's segment below the stricture. It doesn't add much time to the procedure and that IMca could have been spotted earlier!
During a Barrett's surveillance OGD, I notice this small red spot at 6 O'clock.
WHAT IS THE LIKELY HISTOLOGY?
■ Reflux ulcer
I don't think that you get this within Barrett's without dysplasia!
■ LGD
Clear crypt pattern, not that different from surrounding mucosa? Good guess!
■ HGD
Quite possible and would have been my guess IF there was some nodularity associated
■ Early cancer
Impossible as lesion has an organised crypt pattern!
explanation
Previous surveillance samples, 3 years earlier had not revealed any dysplasia. However, that red spot shouldn't be there! A reflux ulcer is unlikely as the Barrett's is there because it protects the food pipe from acid. Of course it does this by developing crypts with Goblet cells which secretes protective mucus (of course the pathologists call this process 'metaplasia'). Early texts usually stated that ulceration is common within Barrett's. In my experience, ulceration within Barrett's only happens when dysplasia develops. With the arrival of dysplasia, you begin to see a disappearance of the Goblet cells and of course when the Goblet cells start to dwindle, so does the protective mucus.
In the bottom zoom image you can see that there is a distinct surface crypt pattern at the site of the red spot. Therefore the cells can't be too disorganised, making cancer unlikely. Actually this turned out to be a spot of LGD. I would have guessed HGD/IMca (pathologists struggle to tell the difference) if there was a visible nodule at the site of the red spot. Isn't it interesting that even at the very earliest stage of dysplasia, the unstable cells signal the need for more oxygen to nearby vessels?
This patient was undergoing a gastroscopy for iron deficiency anaemia. A small ulcer is found in D2.
WHAT IS THE LIKELY AETIOLOGY?
■ Peptic ulcer
Statistically probably most likely diagnosis
■ Pill ulcer
Yes, but what pill?
■ Adenoma
Often do appear depressed here (IIc lesions) but not in this case
■ Early cancer
Early duodenal cancer usually look like sessile adenomas or, less commonly like indurated ulcerated lesions
explanation
If it wasn't for the somewhat odd, elongated appearance of the ulcer, it wouldn't seem odd. However, the only clue to the aetiology is that yellowish appearance. You may be familiar with 'iron pill gastritis' but can you get iron pill duodenitis? Yes you can! It has even been reported in the hypopharynx and the oesophagus. Those dark spots on the histology slides are crystalline iron deposits are easy to spot for the pathologists.
Of course, ferrous sulphate (Fe2+) tablets is the non-toxic form of iron (naturally). However, the tablets can produce mucosal inflammation if the iron becomes oxidised to Ferric iron (Fe3+). You may remember from medical school that most dietary nonheme iron is in the toxic, oxidized form of ferric iron (Fe3+). To absorb iron it first needs to be reduced, in the presence of acid, to ferrous iron (Fe2+). After this, the iron is easily transported across the enterocytes via a divalent metal-ion transporter 1 (DMT1) protein. Here is a link to an open access article if you want to brush up on iron absorption. Naturally, the treatment is to change to the liquid form of iron supplement which is much less toxic to the mucosa than solid iron tablets. This is an elderly patient undergoing an OGD because of IDA (iron deficiency anaemia). A lesion catches my eye on the anterior gastric wall WHAT IS THE LIKELY HISTOLOGY?
■ Gastric xanthelasma
The colour is suggestive and gastric atrophy would be the link but it's not quite right...
■ Healed GU scar
But how about that funny crypt pattern?
■ Gastric adenoma
Yes, doesn't this look like a tubular adenoma?
■ Early gastric cancer
Wouldn't the crypt pattern then be very disorganised or perhaps very small?
explanation
The pale colour is odd and reminiscent of gastric xanthelasma which as you know is linked with gastric atrophy which is the likely cause of this patients IDA. However, when I zoom in on the area, the crypt pattern is different here. Of course, this does not fit with a xanthelasma or a scar from a healed gastric ulcer (GU) either for that matter. Interestingly, almost everyone thought that this was an EGC. However, THERE IS a distinct crypt pattern in the centre of the lesion. Furthermore, the lesion isn't red. Remember that cancers encourage the growth of small irregular capillaries which gives them a red colouration. Finally, it doesn't have the typical flat-elevated with a central depression (IIa+IIc) growth morphology. Therefore, your first guess should be a gastric adenoma! This is actually a gastric tubular adenoma which we found in an elderly frail patient with atrophic gastritis some 10 years ago. As she had some comorbidities and it was only harbouring LGD, we decided to keep an eye on the lesion on a yearly basis. The risk of progression is supposedly only 5% with tubular adenomas in the stomach. In contrast, villous adenomas are much more likely to progress (40%). The BSG gastric polyp guidelines have the references if you want to look this up. Of course, the issue is not entirely clear-cut as risk of progression also increases with the size of the lesion (and this is probably 2cm in size) and also with age (patient is now 86 yrs). In some ways, making an initial decision to either 'attack' or 'abort' would be easiest. After all, regular surveillance drains valuable resources and leaves you open to the possibility that at some point in the future, the patient is no longer a candidate for anything more invasive than a haircut but now the lesion under surveillance shows evidence of progression. Then your patient could well ask the legitimate question why you didn't go ahead when he was younger and fit enough but instead wasted his time with pointless surveillance?! My own preferred way to navigate this minefield is to openly discuss the three options with the patient;
I often wonder if its the personality type which dictates what patients prefer. Perhaps, those who think 'my glass is half empty' usually want to have their lesion resected immediately whilst people who regards their 'glass to be half full', prefer to hope for the best and get on with their lives? |
Categories
All
|