|
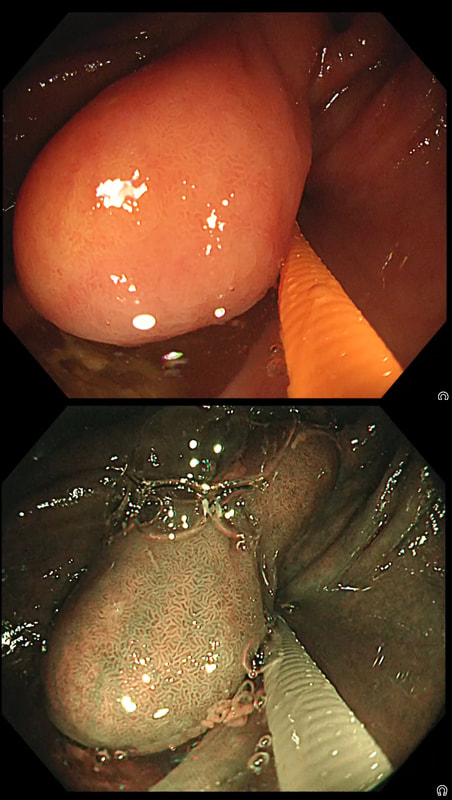
This sizeable polyp was discovered at the ileo-caecal valve and was referred for resection. Samples have not been taken to avoid tethering down making the endoscopic resection uneccessarily difficult. HOW WOULD YOU APPROACH THE LESION?
■ Back off and take some samples
Yes, and perhaps request a CT!
■ Attempt an EMR
You first need to decide what this is!
■ Consider removal by ESD
Can't be adenomatous, it's growing out of the TI!
■ Underwater EMR
Would also be ill advised
■ Refer for surgery
If this is what you think it is, then Yes!
explanation
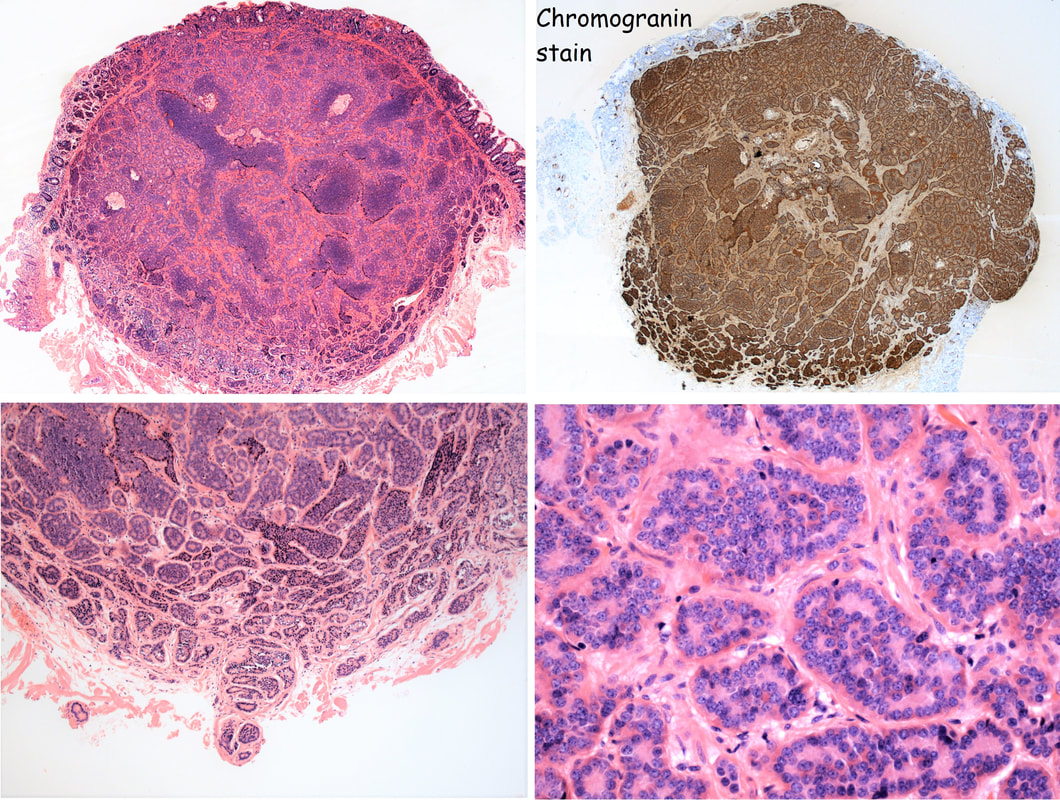
In most cases, I would say 'if it lifts it will shift'. However, in this case I wouldn't bother with a test-lift. The reason is that the thing is growing out of the terminal ileum. You don't get adenomatous polyps growing out of the TI! This must be something else! In fact the true lesion may be larger than the red nipple-like polyp. Even though there are no large 'tell-tale' vessels running up it's side, the only thing of this size, growing out of the TI, is a NET! A lymphoma was my second guess. TI NET's are often bad news and should be considered for surgical resection. There is another odd thing about NET's growing in the terminal ileum. The WHO grading system doesn't seem to relate to the aggressiveness of the lesions behaviour ! This was only WHO grade I (proliferation index was only 1.8%) but on a full analysis after the right hemi-colectomy, the NET was found to be a invading into the muscle propria layer and with metastatic deposits in 2 out of 12 resected lymph nodes (T2,N1) as well as ulcerated deposits of NET in the nearby pericolic fat on the serosal surface. The moral of the story? In the terminal ileum, 'well differentiated NET' doesn't mean that it's well behaved! This 75 year old man underwent a CTC because of a change in bowel habit which has confirmed a large caecal polyp. The patient has been referred for a snare polypectomy. WHAT WOULD YOU DO NEXT?
■ Abort the procedure and reassure the patient
Absolutely!
■ Take a full set of samples
Uneccessary and they will only show normal mucosa
■ Remove the polyp by EMR
Foolish!
■ Remove the polyp by ESD
Idiotic!!!
explanation
The location and the 'pillow sign' tells you that this lesion is a lipoma. We know from Shrisha Hebbar's Podcast that the ICV is a high risk location for any attempt at removing lipomas. He mentions a patient of his who presented with acute small bowel obstruction due to engorgement of an ICV lipoma after the placement of an Olympus ligation.
Furthermore, you wouldn't of course go ahead with an attempt at resecting a lipoma without due consideration of indications. How long has the patient had symptoms? Are they getting better? Are symptoms likely to arise because of this soft and floppy lesion. Probably unlikely and statistically speaking, this elderly patient is probably far more likely to have a change in bowel habit due to constipation. By the way, please take notice of the odd looking mucosal crypt pattern which is reminiscent of a TVA! This is the normal crypt pattern at the ICV at the transition to the villous surface in the terminal ileum! Monz found this lesion in the terminal ileum. WHAT IS THE MOST LIKELY DIAGNOSIS?
■ Hyperplastic polyp
Nope, those are very rare in TI
■ Adenomatous polyp
Uncommon in TI and there are no adenomatous crypts!
■ Neuroendocrine tumour
Perhaps the most common lesion in TI with those typical little vessels!
■ Small leiomyoma
Could be but those little vessels say otherwise
■ Small GIST
Must exist but I've never seen one!
explanation
At diagnostic colonoscopies, I do try to intubate the terminal ileum. Not to 'practise' but to detect pathology such as this rare lesion at an early stage! These do have a real malignant potential and in fact usually present late with bowel obstruction.
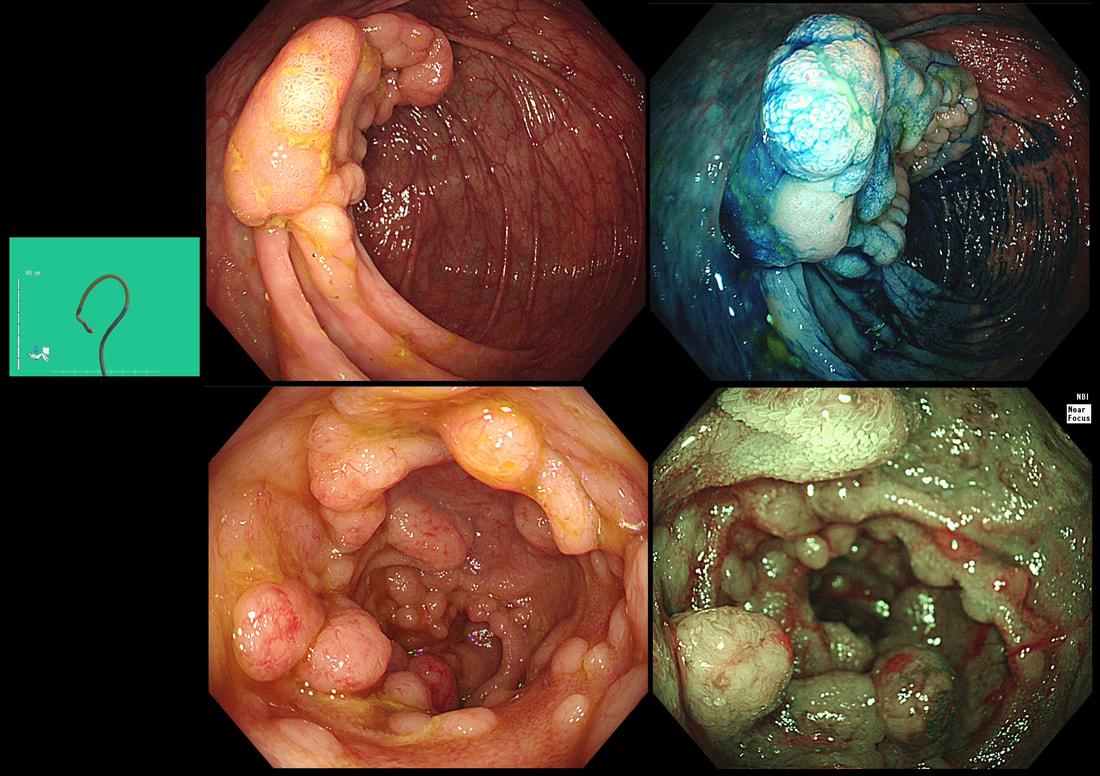
The tell-tale sign are those tiny vessels climbing up around the edges of the polyp and the pale appearance. Of course, this is a terminal ileal NET! The lesion was removed by Monz Ahmed and histology confirmed that it was an NET. Of course, the MOST IMPORTANT issue is the WHO Grade of the lesion. This is because small bowel NET's (excluding the duodenum) are often malignant. The lesion was WHO Grade I (i.e. 1-2% mitotic figures only) which is reassuring but a CT is probably still warranted to look at those nearby lymphnodes. By the way, in the histology below, you can see how close the lesion is on the abutting deep edge. This is the common finding after your endoscopic removal and can be disconcerting. Studies have reported that if you resect lesions using a 'banding device' you can usually get a confirmed (but shallow) clear deep margin. However, neither Monz or I would use a banding device in the terminal ileum. The muscle propria layer is too thin and you are likely to end up with a full thickness resection if you tried. 'Banding resections' are probably best reserved for the oesophagus, stomach or colorectum! This patient was undergoing colonoscopy because of abdominal pain, weight loss and suspected thickening of the terminal ileum seen on CT WHAT IS YOU ENDOSCOPIC DIAGNOSIS? a) Crohn's disease b) Adenocarcinoma c) Lymphoma d) Neuroendocrine tumour e) Tuberculosis explanation
Endoscopically, there appear to be 'nodules' arising from below the overlying mucosa. When I first showed this case, almost everyone correctly identified this as a case of lymphoma. Of course, MALT lymphoma in the stomach looks completely different with thickening and reddening of the gastric mucosa, usually with ulceration of the surface. The reason why this looks entirely different to a gastric MALT lymphoma is because it is a completely different type of lymphoma! Histologically, the submucosal nodules were made up of small to intermediate sized lymphoid cells clusters, forming solid sheets and balls. This is the classical endoscopic appearance of a Mantle Cell Lymphoma (MCL). MCL is a type of non-Hodgkin's lymphoma which arise within the 'mantle zone' that surrounds normal lymphoid follicles. It's presumably for this reason that endoscopically it looks like gross case of nodular lymphoid hyperplasia. It's not a 'good lymphoma' as median life expectancy is only 6-7 yrs. In this patient, a CT confirmed that there were large nodes both above and below the diaphragm. Although he had no symptoms our haematologists have started treatment with 'Ibrutinib' to reduce the risk of small bowel obstruction. From today, you will all recognise the typical endoscopic appearances of a MCL ! |
Categories
All
|