|
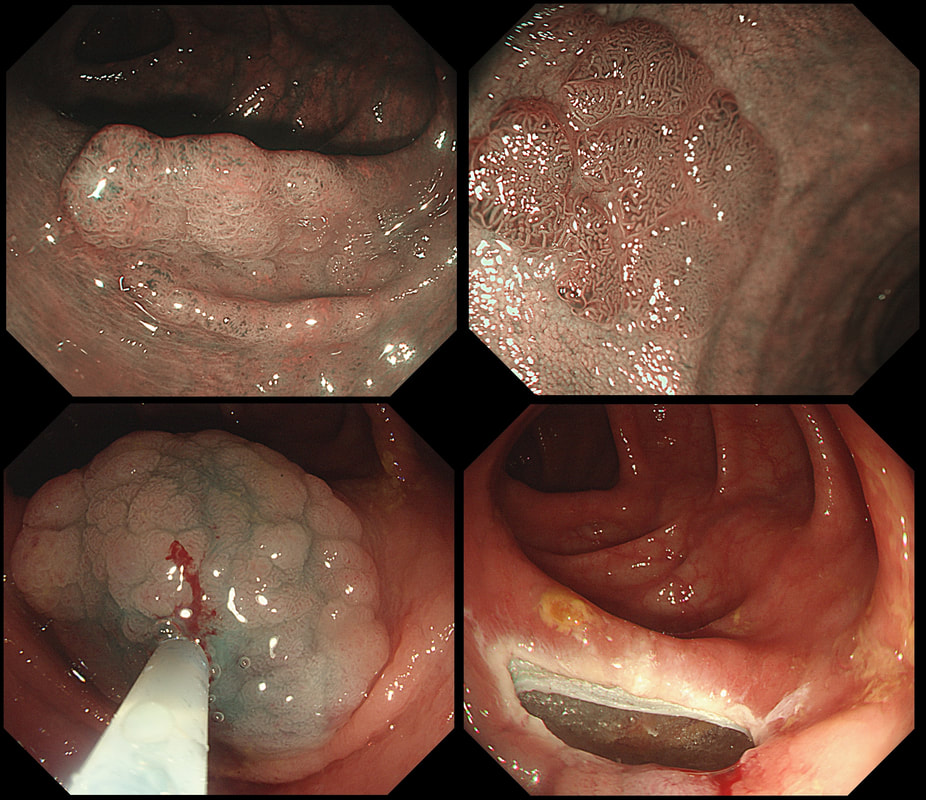
This polyp was found in the transverse colon in a patient with long-standing ulcerative colitis. WHAT WOULD YOU DO NEXT? a) retrieve the polyp and look for other polyps b) obtain 4 samples from the nearby mucosa c) apply APC to the EMR edges d) tidy the edges up with a cold snare e) apply clips Explanation
That hole isn't right! More often than not, this is how a perforation looks immediately after polypectomy. As a beginner you may think that you should be able to see the peritoneum but that would be the exception. Must admit that I was surprised to see this perforation. The lift seemed to be good and I didn't use a 'super-stiff' snare. Perhaps it had something to do with the fact that the patient had colitis? Because the 'cutting' should have taken 6-7 seconds but took about 12 seconds, I did expect 'trouble' and had started to suck air out of the colon before the snare cut through completely. Fortunately, the colonic lumen is not deflating as the perforation is close to the omental reflection. We will have a few minutes before the patient starts to become uncomfortable. Spend those minutes well !!! I applied 10 clips. The colon was clean and I was confident that there was no peritoneal contamination. Of course, this is one of the reasons why your polypectomy site should be as dry and clean as possible before you step on that yellow pedal! There was no pain and after a couple of hours in recovery and I discharged the patient with verbal and written instructions to return to A&E if pain developed later. The patient was fine. Can I reassure you that every patient will be fine after closing a perforation by clips? Of course not! You need to follow your instincts and your local protocols and of course be able to defend your decisions. Naturally, the particulars of the actual patient is very important. For example, an elderly patient or someone living alone should probably not be discharged. After all, sepsis can develop quickly and the patient may soon be in no fit shape to call for help. |
Categories
All
|