|
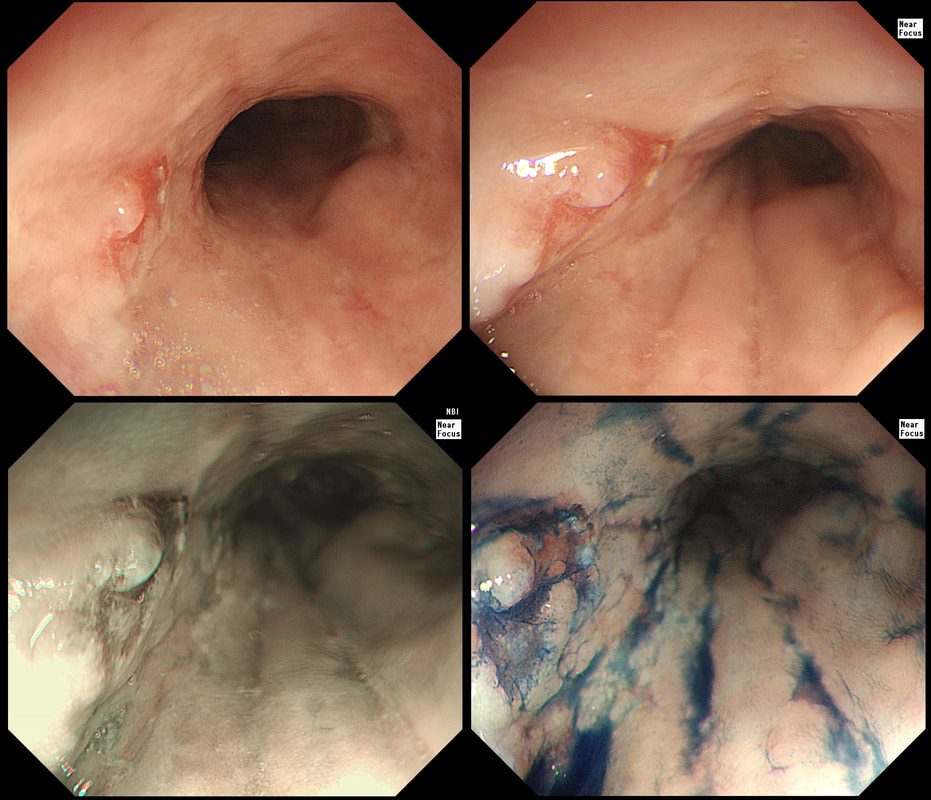
A year ago, this patient underwent RFA for a C5/M6 Barrett's harbouring HGD.
WHAT IS THE MOST APPROPRIATE MANAGEMENT?
■ APC ablation
INCORRECT, the lesion is NOT FLAT!
■ RFA
INCORRECT, because the lesion is too worryingly nodular
■ EMR
CORRECT, the only way to make sure!!!
explanation
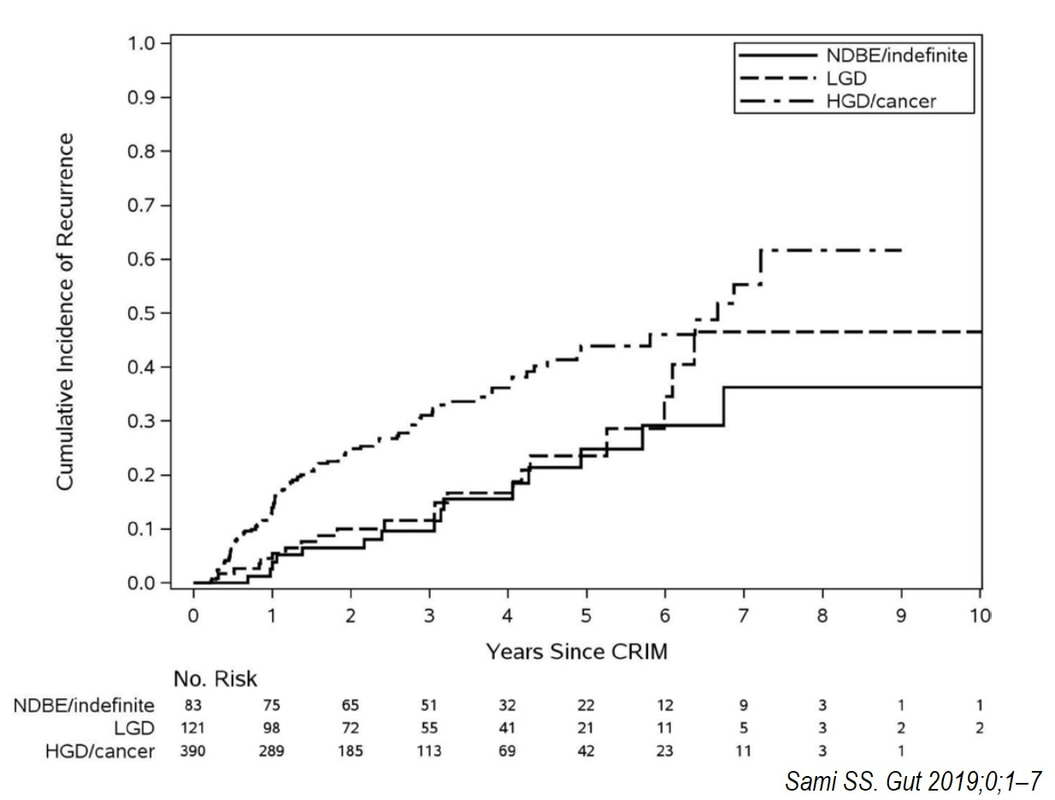
This is the problem with RFA, it doesn't last forever! After 5-6 years, about half your patients will have relapsed. Predictably, it's the patients with the most unstable changes who are the most likely to relapse (see graph below from Dr Sami's landmark paper). This is the reason why surveillance at 12 month and then 3 yearly is recommended by the BSG when the 'index histology' was LGD. However, after HGD or IMca, surveillance after 3 months, 6 months and then annually is recommended. Click here to read those recommendations in full.
Endoscopically, it can be difficult to spot a small rim of Barrett's returning, which over time slowly pushes the squamo-columnar junction proximally. In most cases, this is how Barrett's return over time. It's for this reason that we advice taking 4 biopsies from the columnar side of the SCJ'n. If your pathologists report dysplasia in any of these samples, a "top-up" RFA may well be indicated. Less commonly patients develop a nodule emerging from the 'neo-squamous mucosa' as in this case. Clearly you need to resect this for a full histological analysis. Ablation would be like sweeping it under the carpet! The nodule was removed by EMR and histology revealed an intramucosal cancer! Rather worrying that this patient's disease has in some sense, 'progressed' after RFA. Prof Rebecca Fitzgerald's group at Cambridge has shown us that the DNA is pretty thoroughly mashed up by the time the mucosa looks dysplastic down a microscope. Is it really possible for RFA to 'clean up' and remove all those chromosomal translocations ? |
Categories
All
|