|
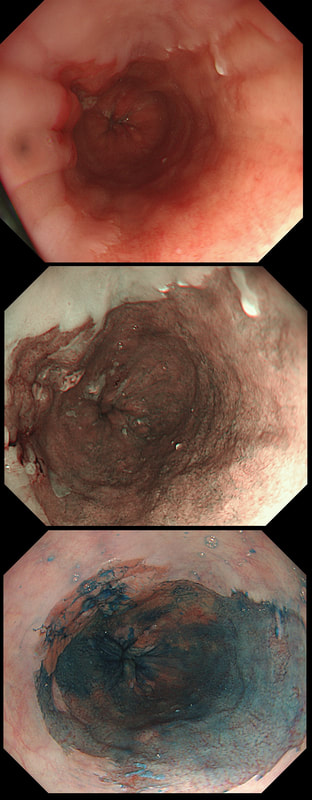
This is a C2M4 Barrett's under surveillance
WHAT IS THE LIKELY HISTOLOGY?
■ Non-neoplastic Barrett's
Nodularity within Barrett's is always bad!
■ LGD
Visible nodularity is never truly just LGD
■ HGD/IMca
A good guess but you are missing something!
■ Invasive cancer
Yes! That small ulcer is the spot of invasive cancer!
explanation
Of course you should initially scrutinise the right-hand part of the Barrett's between 12 and 5 O'clock or so. Furthermore, dysplasia is most common in the distal rather than proximal Barrett's. However, in this case the subtle nodularity is situated in the 11 O'clock position. That is why I call this an 'unusual case' of Barrett's
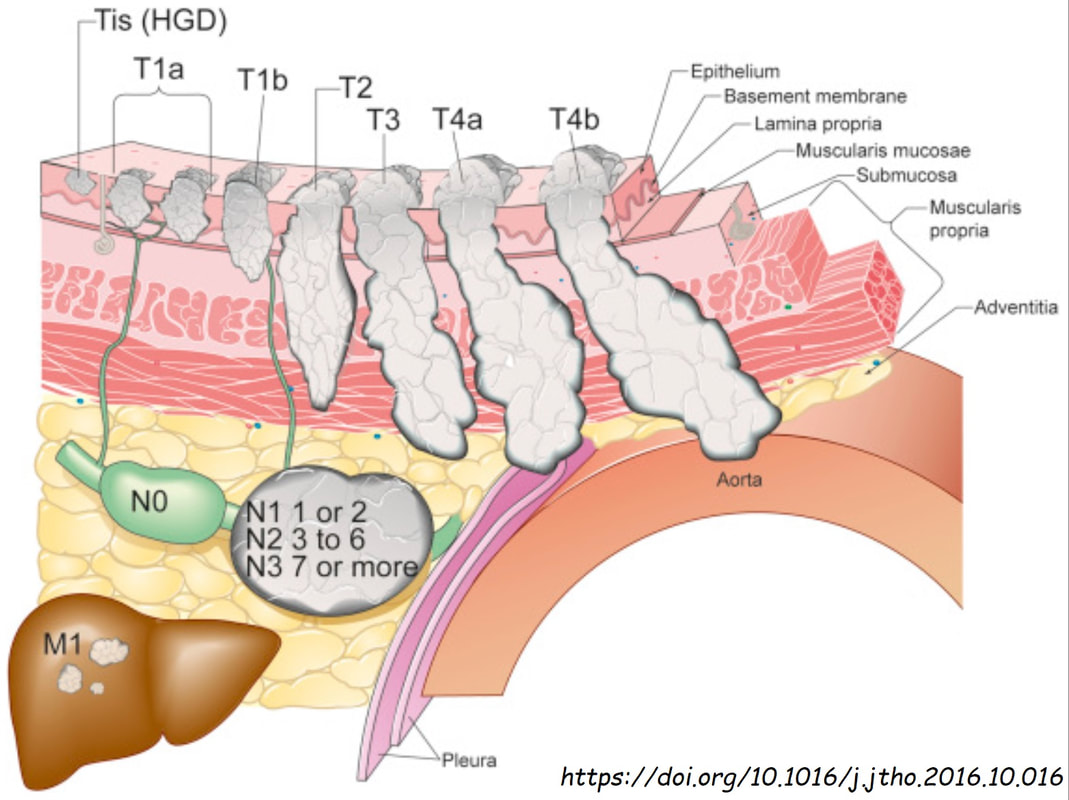
I don't think that LGD is visible endoscopically or possible to recognise even by AI systems. However, in this case there is a definite nodularity and HGD/IMca seems the most likely diagnosis. However, worryingly there is a small depression in the centre of the lesion (seen best on NBI) without any crypt pattern at all. That is the location of the poor differentiation and invasion below the muscular mucosa. Furthermore, biopsies revealed LVI and the patient subsequently had chemoradiotherapy (CRT). CRT is a great option in elderly patients but I do worry when young patients opt for CRT. This is because they are at high risk of developing further lesions and they have decades of life expectancy ahead of them for this to happen. The ultimate staging was T1b, N0 disease. I've attached a reminder about TNM staging because it's easy to forget it unless you see it every day!
|
Categories
All
|