|
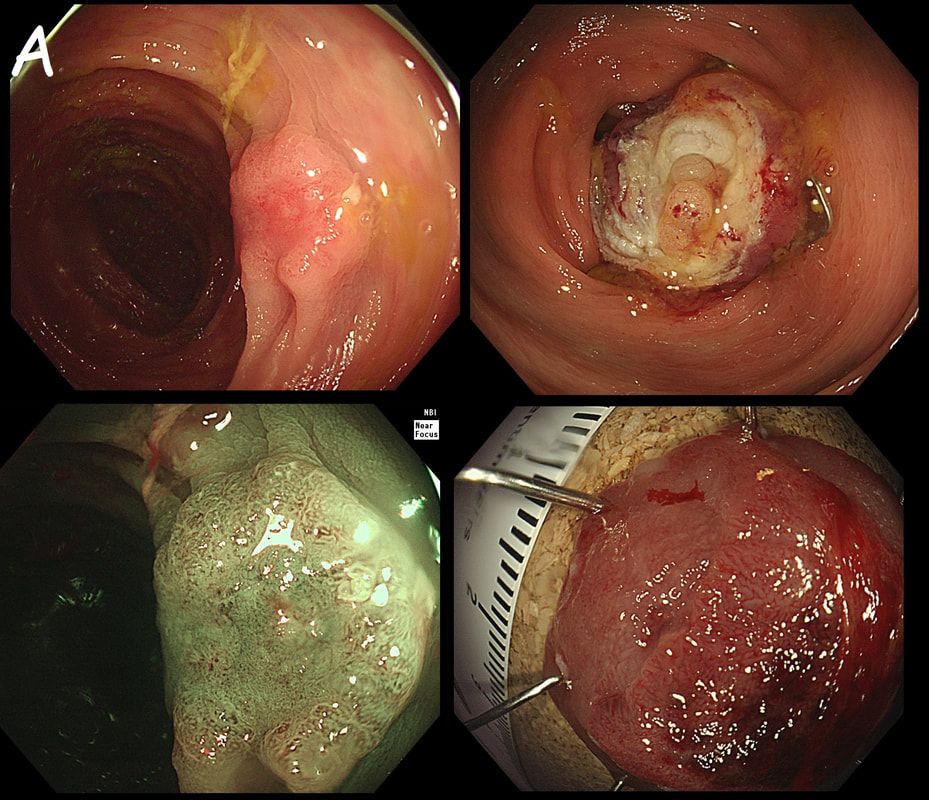
The lesion above is removed 'full thickness' and turns out to be an sigmoid carcinoma extending up to, but not involving the muscle propria layer (i.e. it's a T1 cancer with sm3 invasion). Histology reports clear margins but when the patient returns for a 'site-check' endoscopy, the nodule below in photograph B is found at the resection site ...
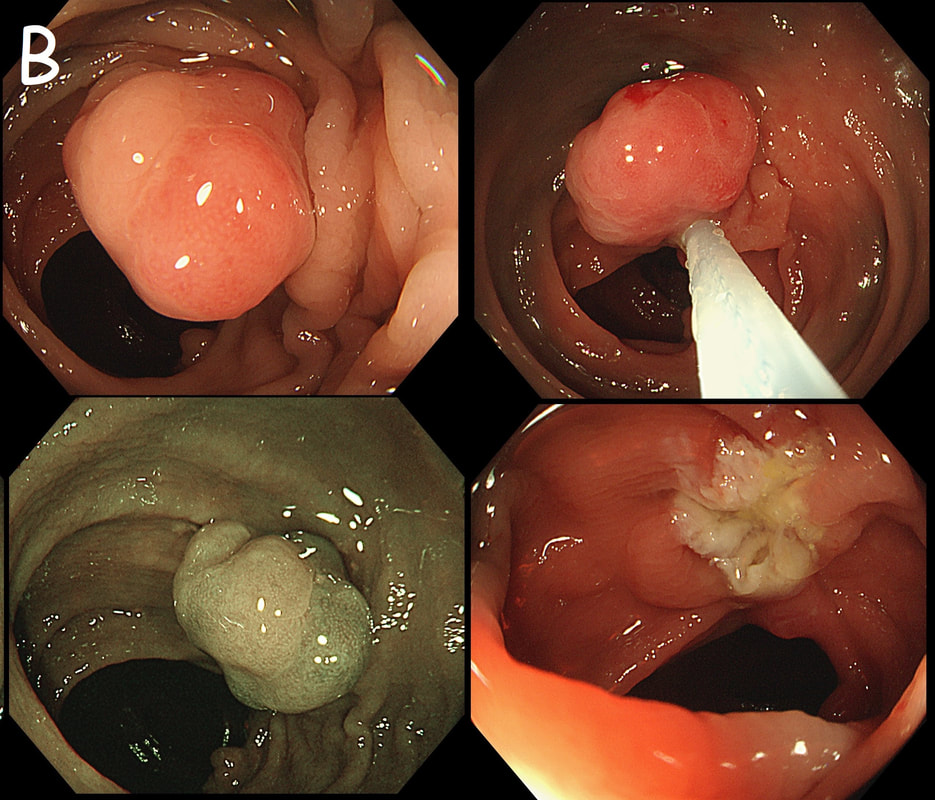
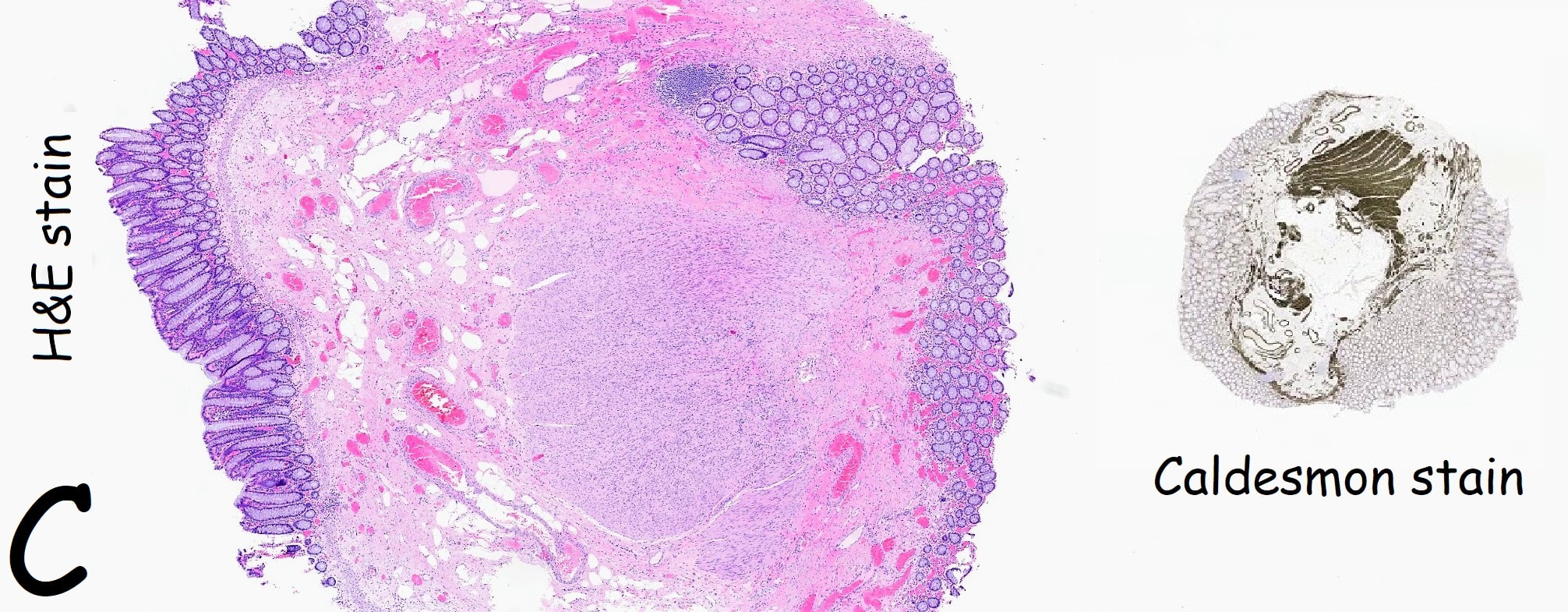
The mysterious nodule is removed and sent for analysis (Histology below as photograph C ) .
WHAT IS THE DIAGNOSIS?
■ Granulomatous/inflammatory reaction
Doesn't look like it!
■ Mucosal prolapse reaction
Yes, what else could it be!
■ Local recurrence of adenoma
Doesn't look adenomatous!
■ Local recurrence of carcinoma
Could be a concern, perhaps submucosal deposit but histology reported clear margins ...
Explanation
Endoscopically, this doesn't look like anything! It doesn't look either inflammatory or neoplastic (i.e. adenoma or cancer). Why then was it removed?! Endoscopically, this looked like normal mucosa but what then is it? To find out, the lesion was removed. I had my suspicions as to what was going on and took great care to close that tiny, unremarkable looking resection site with 4 clips.
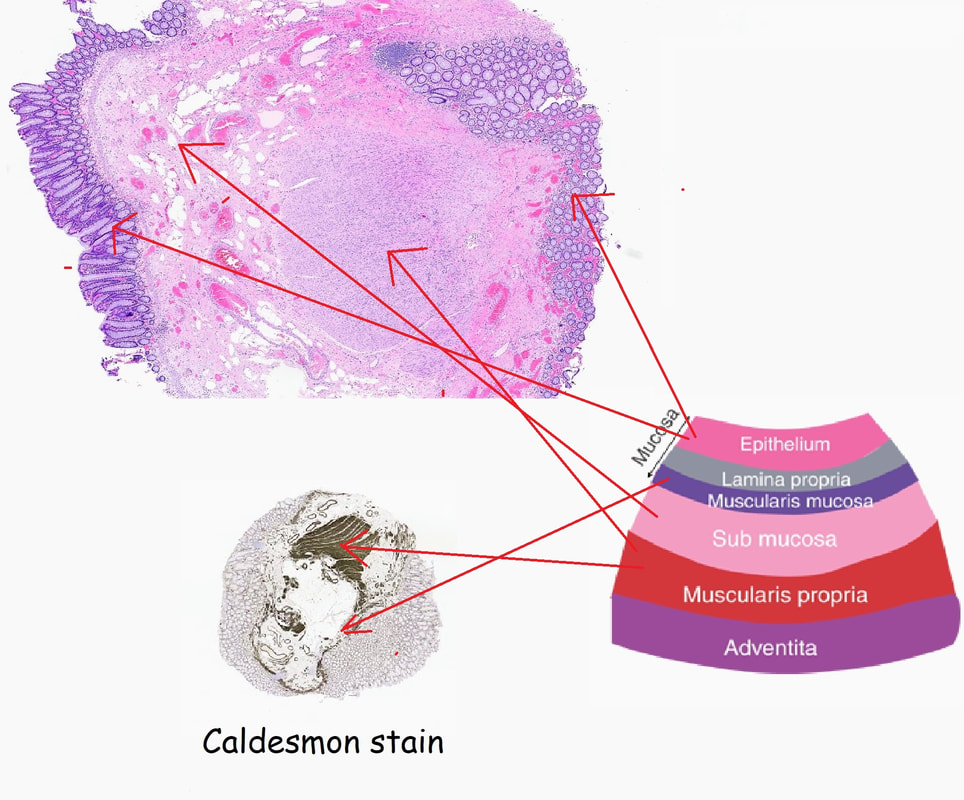
Histology did confirm that this is a full thickness mucosal prolapse at the FTR site. Of course, the point is that if you don't recognise this and resect it, you will end up with a delayed perforation !!! I've attached an annotated histology slide below. As a professional you should understand histology. By the way, the 'Caldesmon stain', shows up muscle. That large grey blob is of muscle propria in the centre of the 'polyp' and the thin grey layer around the periphery, just below the surface epithelium (the polyp is cut in a horizontal manner), is 'muscularis mucosa'. |
Categories
All
|