|
Previous biopsies have confirmed that this rectal polyp harbours TVA+HGD. It's removed by piecemeal EMR and at the end of the 2min video clip you see the end result. WHAT WOULD YOU DO NEXT?
■ Place clips
Always clips !
■ Wait for histology
And of course, you have requested an 'urgent report'!
■ Request EUS
Life is too short for EUS!
■ Organise an MRI
For local staging and confirmed T2,N1 cancer
■ Request staging CT
Looking for mets in the Chest+Abdomen+Pelvis - proved negative!
explanation
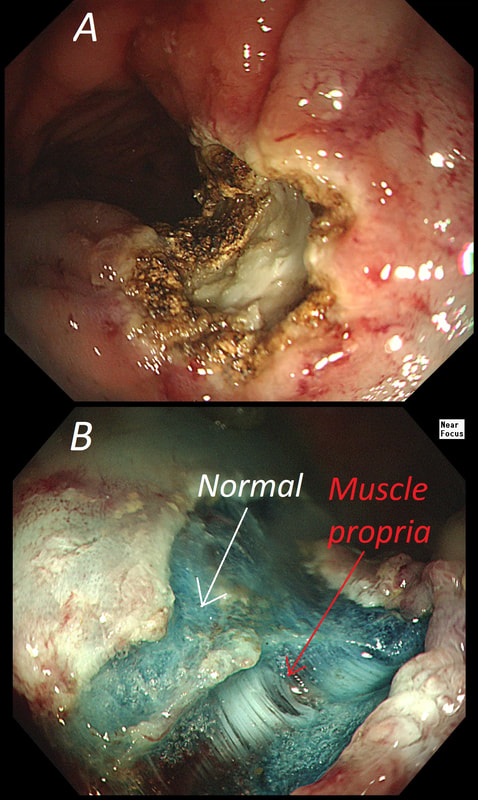
The learning point of this video clip is the EMR defect; it's white (image A) !!! Perhaps the picture below explains it better. Normally my EMR defects are blue (because I mix indigo carmine dye into the submucosal mix). In 'image B' below, the white arrow in the second image shows you what a 'healthy EMR defect should look like. IF you cut too deep, you can see the white, linear fibres of the muscle propria layer (red arrow). Of course this is a warning sign that you MUST carefully close the defect with lots of clips. Actually, next to the tip of the red arrow you can see a black 'micro-perforation' where the full thickness of the muscle layer has been breeched. Naturally, this is were your first clips goes!
Anyway, the mucosal defect in the video clip is just - white, without any linear muscle fibres. This is fibrosis! I have seen fibrosis like this below large sigmoid polyps which have been yanked about with the forceful sigmoid peristalsis. However, the more usual reason for this appearance is that you are looking at the fibrous tissue below a cancer, called 'desmoplasia'. Consequently, if I see a fibrous tissue in the base of the lesion I would do the following: Place clips (because I always do) Fast-track the histology Organise an MRI Request staging CT (chest+abdomen+pelvis) The ultimate diagnosis? Histology confirmed that the polyp was malignant and the imaging (of course requested at the time of the resection), confirmed a T2, N1 carcinoma. A week later, we had a full diagnosis. Unfortunately, the patient turns out not to be a surgical candidate. There is rarely unbridled joy after the endoscopic removal of a CRC ... |
Categories
All
|